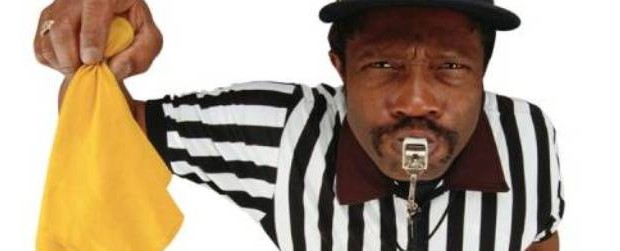
3 Steps to Avoid Penalties for your Eligible Professionals
By Erin Heilman April 7, 2016 Regulatory Updates: Ambulatory
Hospitals with employed Eligible Professionals and organizations must ensure their physicians remain compliant with PQRS and Meaningful Use reporting.
While PQRS reporting is “optional,” there is a “negative fee schedule adjustment” for those providers who bill Medicare on a CMS-1500 claim form and fail to report PQRS quality measures to CMS. Surprised penalized physicians typically turn to IT for answers about reversing or avoiding these penalties.
The good news is, these penalties are avoidable.
Here are three steps you can take to avoid this issue all together:
- Determine which way your hospital’s eligible professionals will report for these programs: 1) by submitting as individual providers, or 2) through your organization’s group reporting option (GPRO). Select your reporting option no later than June 30, 2016 on the cms.gov web site.
- Educate staff, administrators and clinicians about the requirements and processes for physician reporting. Relying solely on IT staff to report quality is quickly becoming inadequate. Quality staff and practice managers can be instrumental in facilitating the decision-making around PQRS and Meaningful Use reporting, helping to avoid growing penalties.
- Ensure your hospital has certified, quality reporting software installed for your eligible providers. Utilizing a quality reporting solution that is user-friendly, configured to pull data directly from your certified EHR and that displays near real time data, helps providers meet their reporting requirements.






Add a comment