eCQM Submissions: Rejections and Mismatches 101
By Kristen Beatson, RN April 6, 2018 Regulatory Updates: Hospital
Did your hospital have eCQM submission rejections or mismatches in 2017? Don’t fret. There’s a solution.
But wait. What does it even mean if you have rejections or mismatches? Let’s break it down. A patient’s QRDA file (Quality Reporting Document Architecture) gets rejected when the agency—CMS or The Joint Commission—finds an error, either a technical issue like an incorrect file format or a clinical data issue, and the error prevents them from accepting the file into their system.
Rejected files need to be corrected and resubmitted for submissions to be considered complete and successful. Medisolv assists hospitals in resolving rejections by reviewing the error, file and associated data, using various reports provided by QualityNet and The Joint Commission. Once the review is complete, we have a better understanding of what the error is and how to fix it for resubmission.
A mismatch or misalignment, on the other hand, happens when the agency places a patient in a different population than the hospital’s eCQM reporting tool. While mismatches aren’t required to be corrected, it’s always a good idea to evaluate, understand and correct them, if possible, to ensure that the data submitted is an accurate reflection of the quality of care in your organization.
Now that you know a bit more about rejections and mismatches, let’s take a look at our top ten 2017 eCQM rejections and mismatches from the CMS Inpatient Quality Reporting (IQR) program and The Joint Commission ORYX® program below. Did your hospital have similar experiences?
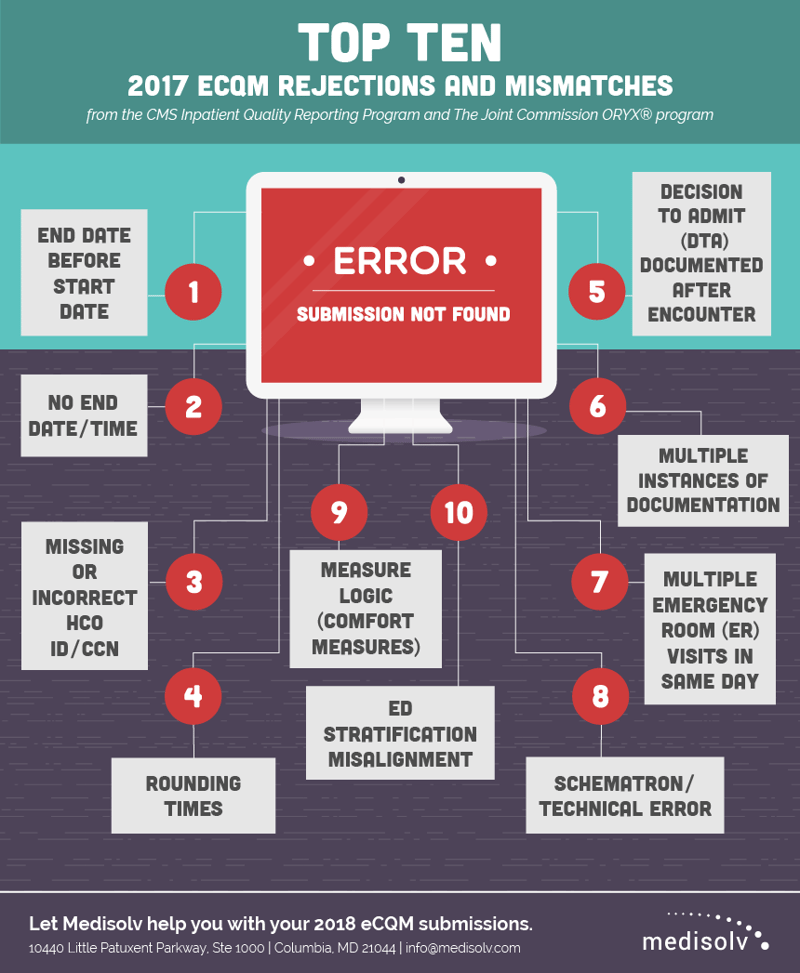
- End date/time before start date/time
This top rejection typically occurs when the discharge or depart time for a hospital visit is either incorrect or not entered. In several EHRs, we found that the field automatically defaults to midnight when the time is not entered, potentially causing a rejection.
- No end date/time
Did you enter the end date and time? Most eCQMs require an end date/time in addition to a start date for all data elements, so save your hospital a rejection by confirming that these are captured and included in the submission data.
- Missing or incorrect HCO ID/CCN
Be sure to double, triple and quadruple check your HCO or CCN ID before submission. You’ll get rejected for not including one—and even for any typos.
- Rounding times
Depending on the specific data element you choose within the eCQM logic, date and time stamps are required to be rounded in seconds, minutes or hours. These rounding requirements are set by the logic and vary between which entity you are submitting to, i.e. CMS or The Joint Commission. If these are not properly rounded, a mismatch can occur.
- Decision To Admit (DTA) documented after encounter
If your hospital is completing documentation well after a patient has been discharged from your facility, you’ve got a problem. Womp, womp. A DTA that’s documented days or weeks after a hospital visit will potentially cause rejections and won’t be any good for a successful or accurate eCQM submission. The DTA documentation (as with most eCQM documentation) should always occur during the patient’s actual stay in the hospital.
- Multiple instances of documentation
Did you document the patient’s C-Section multiple times? Oops, GO BACK! When a procedure or DTA is documented more than once, CMS, The Joint Commission and your submission vendor will have no way of knowing which is accurate. If the incorrect instance is selected, a mismatch can occur.
- Multiple Emergency Room (ER) visits in same day
This error happens when a patient who had been in the ER comes back a second time within that same day. Because of the timing within the logic for that measure, both of those ER visits may be evaluated in the submission. Misalignment looms if the agency or vendor takes the Arrival Time for one visit and pairs it with the DTA for the second instance.
- Schematron/Technical Error
Fortunately, schematron and technical errors can usually be detected at the beginning of the submission process and resolved quickly by your submission vendor. The key is to test early so it doesn’t trip you up at the end!
- Measure logic (comfort measures)
In 2017, a flaw in the Stroke 5 eCQM logic was allowing comfort measures to be evaluated even if they were documented for a visit that occurred AFTER the qualifying visit. This resulted in the patient being excluded incorrectly in 2017 and a mismatch in results. The logic has been fixed for 2018.
- ED Stratification misalignment
Take some time to carefully review your ED measures before submission, particularly the Initial Patient Population (IPP), which should be the same for each strata. If you come across differences, you can review the report details and work with an (awesome) eCQM vendor like Medisolv to help resolve those differences.
C’mon, don’t just throw your hands up in the air. Take action! Resolving your rejections and mismatches is essential both for meeting your eCQM requirements and for improving your hospital’s quality of care.
Rejected? That was so last year. Let Medisolv help you with your 2018 eCQM submissions. When you use Medisolv’s ENCOR software, you not only get a product that gives you up-to-date information on your eCQM performance, you also get a team of experts who submit your eCQM data and work to resolve these rejections, so you don’t have to. Find out more, email us at info@medisolv.com.
Get Ahead and Improve Your QualityMedisolv Can Help We've seen some big changes in the CMS eCQMs. With Medisolv as your partner we help guide you through every new change along the way. Talk with us about how we can help you track and improve your quality performance. Blog Post: "What Makes Up an eCQM?" |






Add a comment