MIPS 2021 Requirements

What’s the biggest change to MIPS in 2021?
To the individual clinician, it’s that they have greater control of their score and incentive money than before.
That’s because CMS changed the previous rule that eligible clinicians reporting through an APM (like an ACO) get the APM’s score regardless of individual performance. This year, clinicians can report their own information and CMS will take the clinician’s highest score, whether that’s in an ACO, or as part of a group, or even their own individual performance. Translation, you may be able to make more money than before.
To an ACO, the big news is two-fold. Firstly, all ACOs that are part of the Medicare Shared Savings Program (MSSP) must use a brand-new framework to report for their practices. Secondly, the CMS Web Interface submission method that ACOs and clinician offices have used to report MIPS to CMS is going away in 2022. That means by the beginning of next year, ACOs and clinician practices need to figure out another way of reporting their practice’s data whether that’s reporting MIPS CQMs, eCQMs or a combination. Figuring out data aggregation will be key for ACOs this year.
Let’s dive into the details.
Understanding MIPS Participation Eligibility
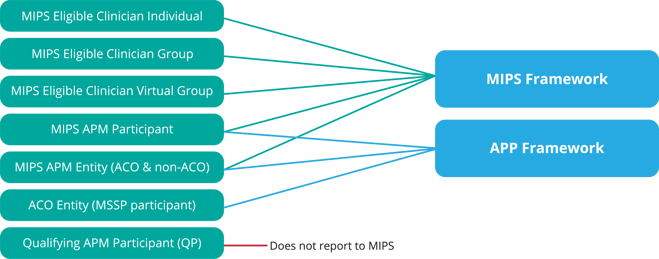
Before we begin, let’s review the types of MIPS participants to understand your options better.
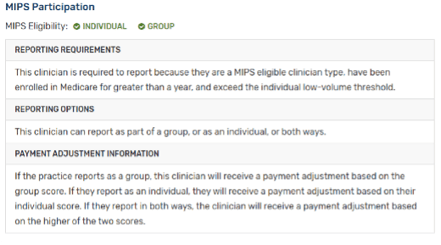
CMS puts Eligible Clinicians into one or more categories.
- Not eligible
- Clear enough.
- MIPS Eligible Clinician Individual
- As an individual clinician you are required to report to MIPS.
- MIPS Eligible Clinician Group
- As an eligible clinician you are required to report to MIPS, and you are able to report as part of a group. Groups are made up of clinicians who all bill with the same Tax ID (TIN).
- MIPS Eligible Clinician Virtual Group
- As an eligible clinician you are required to report to MIPS, and you are able to report as part of a virtual group. Virtual groups must be comprised of 10 or fewer Eligible Clinicians and, as a group, exceed the low-volume threshold.
- Qualifying APM Participant (QP)
- This clinician is a part of an Advanced APM Entity and therefore does not have to report to MIPS and automatically receives a +5% payment.
- This clinician is a part of an Advanced APM Entity and therefore does not have to report to MIPS and automatically receives a +5% payment.
 MIPS APM Participant
MIPS APM Participant
- This clinician is part of an APM Entity, but it is not an Advanced APM, therefore they still must submit data for MIPS.
- This clinician is part of an APM Entity, but it is not an Advanced APM, therefore they still must submit data for MIPS.
One more thing I’ll add here is that those participation statuses apply to the NPI associated with each provider. We will also be referencing APM Entities in the information below. An APM Entity is responsible for reporting to the MIPS program on behalf of their participants. There are Advanced APMs which take on some form of financial risk. These organizations do not have to report to MIPS. There are other APM Entities which are not designated as advanced. ACOs make up a good portion of these types of organizations.
As an individual clinician you may have relied on your ACO to report on your behalf.
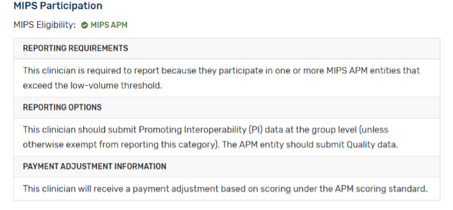
To find out your participation framework you must check your eligibility on the QPP website.
CMS released a brand-new reporting framework
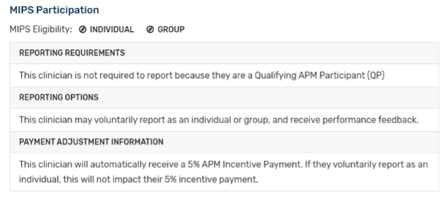
Once you know your participation status, you will understand which framework you can use for submission. There are two MIPS frameworks in 2021, the Traditional MIPS Framework and the APM Performance Pathway (APP) Framework.
Traditional MIPS Framework
This is the usual MIPS framework made up of four categories and a composite score.
APM Performance Pathway (APP) Framework
The APP Framework is new and is available to MIPS APM entities and required for ACOs if they are part of MSSP.
Here is a matrix of which framework you can report to, based on your status.
Each framework has slightly different requirements and different category weights.
MIPS Framework Category Weights
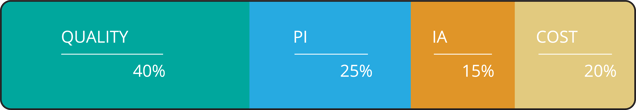
APP Framework Category Weights

Now before we move on to the category requirements, we need to clarify one more definition, collection types.
Defining MIPS Collection Types
Collection types are the way you report the data to CMS. You can think of them like measures. There are six collection types in 2021.
- eCQMs (Electronic Clinical Quality Measures)
- MIPS CQMs (previously called Registry measures)
- QCDR measures (Qualified Clinical Data Registry)
- Medicare Part B Claims measures
- CAHPS for MIPS survey
- CMS Web Interface measures
As I mentioned before, CMS Web Interface is going away next year so if this is the primary way you submitted your MIPS measures before, you need to figure out a new collection type for 2022.
Which collection type you can submit depends upon your participation status. For instance, CMS Web Interface measures can only be submitted by groups with 25 or more eligible clinicians.
Now we are ready to review the requirements for each framework.
2021 MIPS Quality Requirements
Traditional MIPS Framework (Non-CMS Web Interface)
Quality Category Traditional MIPS Framework (Non-CMS Web Interface)
- Category weight: 40% of total MIPS score
- Performance Period: 365 days
- Requirements:
- Submit 6 measures one of which is an outcome measure or high priority measure
- Report data for at least 70% of patients who qualify for a measure
- You may use a combo of collection types
- Two administrative quality claims measures are calculated automatically
- CAHPS for MIPS survey
- Measure list
- Quality Measures
- Hospital-Wide, 30-Day, All-Cause Unplanned Readmission (HWR) Rate for MIPS Eligible Groups. This measure is replacing the All-Cause Hospital Readmission (ACR) measure.
- Risk-standardized Complication Rate (RSCR) following Elective Primary Total Hip Arthroplasty (THA) and/or Total Knee Arthroplasty (TKA) for MIPS
- Available Collection Types
- eCQMs
- MIPS CQMs
- QCDR measures
- Administrative claims quality measures (Only small practices may submit quality measures using claims)
- CAHPS for MIPS survey
- Other Considerations
- Submitting the CAHPS for MIPS Survey will count as reporting one High Priority measure. Select five other Quality measures to report, including an Outcome measure if available.
- Case Minimum
- Quality measures must meet the 20-case minimum to be scored.
Traditional MIPS Framework (CMS Web Interface)
Quality Category Traditional MIPS Framework (CMS Web Interface)
- Category weight:40% of total MIPS score
- Performance Period: 365 days
- Requirements:
- Must be a group, virtual group or APM entity (including ACOs) with 25 or more eligible clinicians
- Submit all 10 measures
- Two administrative claims quality measures are calculated automatically
- CAHPS for MIPS survey (Optional)
- Measure list
- Quality Measures
- Diabetes: Hemoglobin A1c (HbA1c) Poor Control
- Preventive Care and Screening: Screening for Depression and Follow-Up Plan
- Controlling High Blood Pressure
- Falls: Screening for Future Fall Risk
- Preventive Care and Screening: Influenza Immunization
- Preventive Care and Screening: Tobacco Use: Screening and Cessation Intervention
- Colorectal Cancer Screening
- Breast Cancer Screening
- Statin Therapy for the Prevention and Treatment of Cardiovascular Disease
- Depression Remission at Twelve Months
- Administrative Claims Quality Measures
- Hospital-Wide, 30-Day, All-Cause Unplanned Readmission (HWR) Rate for MIPS Eligible Groups. This measure is replacing the All-Cause Hospital Readmission (ACR) measure
- Risk-standardized Complication Rate (RSCR) following Elective Primary Total Hip Arthroplasty (THA) and/or Total Knee Arthroplasty (TKA) for MIPS
- CAHPS for MIPS Survey measure
- Quality Measures
- Available Collection Types
- CMS Web Interface measures
- Administrative Claims measures
- CAHPS for MIPS survey measures
APP Framework (Non-CMS Web Interface)
Quality Category APP Framework (Non-CMS Web Interface)
- Category weight: 50% of total MIPS score
- Performance Period:365 days
- Requirements:
- Submit 3 quality measures
- Report data for at least 70% of patients who qualify for a measure
- You may use either eCQMs and/or MIPS CQMs
- Two administrative claims measures are calculated automatically
- CAHPS for MIPS survey
- Measure list
- Quality Measures
- Diabetes: Hemoglobin A1c (HbA1c) Poor Control
- Preventive Care and Screening: Screening for Depression and Follow-Up Plan
- Controlling High Blood Pressure
- Administrative Claims Quality Measures
- Hospital-wide, 30-day, All-Cause Unplanned Readmission (HWR) Rate for MIPS Eligible Clinician Groups
- Risk Standardized, All-Cause Unplanned Admissions for Multiple Chronic Conditions for ACOs.
- Quality Measures
- Available Collection Types
- eCQMs
- MIPS CQM
- Administrative Claims measures
- CAHPS for MIPS survey
- Other Considerations
- In order for ACOs to meet the Shared Savings Program quality performance standard, they must achieve a quality performance score that is equivalent to or higher than the 30 percentile across all MIPS Quality scores.
APP Framework (CMS Web Interface)
Quality Category APP Framework (CMS Web Interface)
- Category weight: 50% of total MIPS score
- Performance Period: 365 days
- Requirements
- Must be a group, virtual group or APM entity (including ACOs) with 25 or more eligible clinicians
- Submit all 10 measures
- Two administrative claims measures are calculated automatically
- CAHPS for MIPS survey
- Measure list
- Quality Measures
- Diabetes: Hemoglobin A1c (HbA1c) Poor Control
- Preventive Care and Screening: Screening for Depression and Follow-Up Plan
- Controlling High Blood Pressure
- Falls: Screening for Future Fall Risk
- Preventive Care and Screening: Influenza Immunization
- Preventive Care and Screening: Tobacco Use: Screening and Cessation Intervention
- Colorectal Cancer Screening
- Breast Cancer Screening
- Statin Therapy for the Prevention and Treatment of Cardiovascular Disease
- Depression Remission at Twelve Months
- Administrative Claims Quality Measures
- Hospital-wide, 30-day, All-Cause Unplanned Readmission (HWR) Rate for MIPS Eligible Clinician Groups
- Risk Standardized, All-Cause Unplanned Admissions for Multiple Chronic Conditions for ACOs.
- CAHPS for MIPS Survey
- Quality Measures
- Available Collection Types
- CMS Web Interface measures
- Administrative Claims measures
- CAHPS for MIPS survey
- Other Considerations
- In order for ACOs to meet the Shared Savings Program quality performance standard, they must achieve a quality performance score that is equivalent to or higher than the 30 percentile across all MIPS Quality scores.
2021 MIPS Promoting Interoperability Requirements
Traditional MIPS Framework
PI Category Traditional MIPS Framework
- Category weight: 25% of total MIPS score
- Performance Period: 90 days
- Requirements
- Submit the 4-5 required measures
- Collect your data in EHR technology with 2015 Edition certification criteria, 2015 Edition Cures Update certification criteria, or a combination of both
- Provide your EHR’s CEHRT ID from the Certified Health IT Product List (CHPL)
- Conduct or review a security risk analysis on your 2015 Edition CEHRT functionality on an annual basis
- Attest to the Prevention of Information Blocking and ONC Direct Review
- Promoting Interoperability Measures
- e-Prescribing
- Support Electronic Referral Loops by Sending Health Information
- Support Electronic Referral Loops by Receiving and Reconciling Health Information
- e-Prescribing
- Optional: Instead of measures 2&3 you may submit the new Health Information Exchange (HIE) bi-directional exchange measure
- Provide Patients Electronic Access to Their Health Information Report to two different public health agencies or clinical data registries for any of the following:
- Immunization Registry Reporting
- Electronic Case Reporting
- Public Health Registry Reporting
- Clinical Data Registry Reporting
- Syndromic Surveillance Reporting
- Provide Patients Electronic Access to Their Health Information Report to two different public health agencies or clinical data registries for any of the following:
- Bonus: Query of Prescription Drug Monitoring Program (PDMP)
-
- If your APM Entity is reporting your quality and improvement activities data, you will still need to submit your Promoting Interoperability data at the individual or group level for traditional MIPS.
- If you do not meet all 5 requirements listed above (or if you do not claim an exclusion) you will receive a total score of zero in this category.
- The Query of Prescription Drug Monitoring Program (PDMP) measure will remain as an optional bonus measure worth <strong>10 bonus points.
- CMS will automatically assign a weight of zero to this category for the following clinician types:
- Nurse Practitioners (NPs)
- Physician Assistants (PAs)
- Certified Registered Nurse Anesthesiologists (CRNAs)
- Clinical Nurse Specialists (CNSs)
- Physical Therapists
- Occupational Therapists
- Qualified Speech-language Pathologists
- Qualified Audiologists
- Clinical Psychologists
- Registered Dietitians or Nutrition Professionals
APP Framework
PI Category APP Framework
- Category weight: 30% of total MIPS score
- Performance Period: 90 days
- Requirements
- Submit the 4-5 required measures
- Collect your data in EHR technology with 2015 Edition certification criteria
- Provide your EHR’s CEHRT ID from the Certified Health IT Product List (CHPL)
- Conduct or review a security risk analysis on your 2015 Edition CEHRT functionality on an annual basis</li>
- Attest to the Prevention of Information Blocking and ONC Direct Review</li>
- Measure list
- Promoting Interoperability Measures
- e-Prescribing
- Support Electronic Referral Loops by Sending Health Information
- Support Electronic Referral Loops by Receiving and Reconciling Health Information
- e-Prescribing
- Optional: Instead of measures 2 & 3 you may submit the new Health Information Exchange (HIE) bi-directional exchange measure
- Provide Patients Electronic Access to Their Health Information
- Report to two different public health agencies or clinical data registries for any of the following:
- Immunization Registry Reporting
- Electronic Case Reporting
- Public Health Registry Reporting
- Clinical Data Registry Reporting
- Syndromic Surveillance Reporting
- Bonus: Query of Prescription Drug Monitoring Program (PDMP)</li>
- Promoting Interoperability Measures
- Other Considerations
- Promoting Interoperability data is only submitted at the individual or group level, not through the APM Entity. For Eligible Clinicians, your PI data is either submitted through QPP or by a third party vendor to CMS. You’ll continue this in 2021. Your calculated PI score is generated from all scores of MIPS eligible clinicians reporting participating in the APM Entity you are part of.
2021 MIPS Improvement Activities Requirements
Traditional MIPS Framework
IA Category Traditional MIPS Framework
- Category weight: 15% of total MIPS score
- Performance Period: 90 days
- Requirements
- Submit one of the following combinations of activities
- 2 high-weighted activities
- 1 high-weighted activity and 2 medium-weighted activities, or
- 4 medium-weighted activities
- Submit one of the following combinations of activities
- Measure list
- Improvement Activity Measures
- Other Considerations
- If you’re a clinician in any APM who is participating in traditional MIPS, you’ll earn half credit (50%) automatically for the IA category. You may submit additional improvement activities to earn a higher score.
- If you are submitting as a group at least 50% of your group's clinicians must attest to completing the same improvement activity for 90 consecutive days. The activity may be completed anytime within the calendar year, as long as each person attesting completes the same activity for 90 consecutive days.
- Patient-Centered Medical Homes
- If you are a Patient-Centered Medical Home and more than 50% of your practices are recognized as a PCMH, you automatically receive full credit for this category.
APP Framework
IA Category APP Framework
- Category weight: 20% of total MIPS score
- Performance Period: 90 days
- Requirements
- If the APM Entity is reporting through the APP, CMS will automatically assign a score of 100% which is applied to all eligible clinicians reporting through their APM Entity.
- Measure list
- Improvement Activity Measures are determined by your APM/ACO.
- Other Considerations
- For APM Entity reporting, at least 50% of the clinicians in the APM Entity must perform an improvement activity for the APM Entity to be able to attest to it.
2021 MIPS Cost Requirements
Traditional MIPS Framework
Cost Category Traditional MIPS Framework
- Category weight: 20% of total MIPS score
- Performance Period: 365 days
- Requirements:
- CMS will evaluate your performance on these two cost measures: Medicare Spending per Beneficiary-Clinician (MSPB-C) and Total Per Capita Cost.
- CMS will also evaluate your performance on these 18 episode-based measures.
- Measure list
- Cost Measures
- Total Per Capita Costs (TPCC)
- Medicare Spending Per Beneficiary-Clinician (MSPB-C)
- Episode Based Measures
- Acute Kidney Injury Requiring New Inpatient Dialysis
- Elective Outpatient Percutaneous Coronary Intervention (PCI)
- Elective Primary Hip Arthroplasty
- Femoral or Inguinal Hernia Repair
- Hemodialysis Access Creation
- Inpatient Chronic Obstructive Pulmonary Disease (COPD) Exacerbation
- Intracranial Hemorrhage or Cerebral Infarction
- Knee Arthroplasty
- Lower Gastrointestinal Hemorrhage (groups only)
- Lumbar Spine Fusion for Degenerative Disease, 1-3 Levels
- Lumpectomy Partial Mastectomy, Simple Mastectomy
- Non-Emergent Coronary Artery Bypass Graft (CABG)
- Renal or Ureteral Stone Surgical Treatment
- Revascularization for Lower Extremity Chronic Critical Limb Ischemia
- Routine Cataract Removal with Intraocular Lens (IOL) Implantation
- Screening/Surveillance Colonoscopy
- Simple Pneumonia with Hospitalization
- ST-Elevation Myocardial Infarction (STEMI) with Percutaneous Coronary Intervention (PCI)
- Cost Measures
- Other Considerations
- CMS requires a case minimum of 35 for the MSPB-C measure and 20 for the Total Per Capita Cost measure.
- CMS also requires a minimum of 10 episodes for the procedural measure types and 20 episodes for the acute inpatient medical condition measure types.
- CMS is adding telehealth services directly applicable to existing episode-based cost measures and the TPCC measure.
APP Framework
Cost Category APP Framework
- Category weight: 0% of total MIPS score
- Requirements
- If the APM Entity is reporting through the APP, CMS will not calculate a Cost score as part of their total MIPS score.
MIPS 2021 Bonus Points
There are many opportunities to get bonus points within the MIPS program.
Improvement Bonus: Up To 10 Points
Clinicians will be rewarded if they demonstrate any improvement to their 2021 Quality score over the prior year (pending there is enough data for comparison).
Electronic Submission: Up To 6 Points
Receive up to 6 bonus points by submitting your Quality measures via electronic submission.
Additional Measure Submission: Up To 6 Points
By submitting additional Outcome (2 points) High Priority measures (1 point) in the Quality category, you can be rewarded up to 6 bonus points.
PDMP Measure Bonus: Up To 10 Points
Report on the Query of Prescription Drug Monitoring Program measure to receive 10 bonus points.
Complex Patient Bonus: 5 Points
For clinicians who work with patients that have more complex cases, CMS will award up to 5 points to account for the additional complexity of treating their patient population.
Small Practice Bonus: 6 Points
An additional 6 bonus points will be added to the numerator of the Quality category for anyone qualifying as a small practice.
MIPS 2021 Score Threshold
To avoid a -9% penalty, you must score at least 60 points.
To be eligible for bonus money you must score at least 85 points (Exceptional Performance Bonus).
Reimbursements
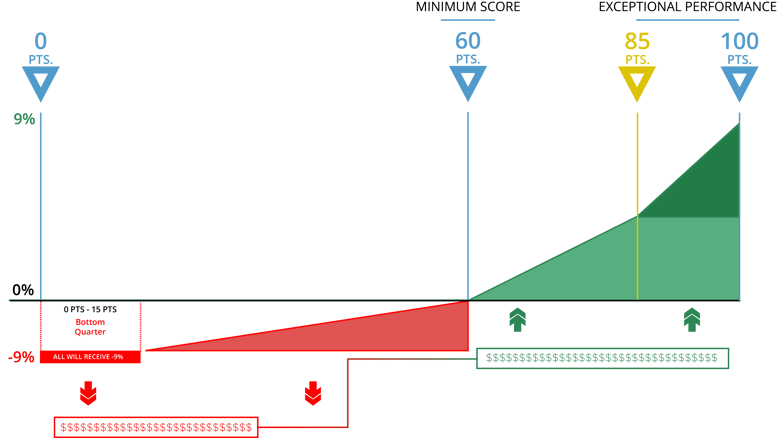
0-15 Points
If your score is between 0 and 15 points in 2021, you will lose -9% from your 2023 Medicare fee schedule (in red above).
15.01-59.99 Points
If your score is between 15.01 and 59.99 points you will receive a reduction to your 2023 Medicare fee schedule between -8.99% and 0%
60 Points
60 points is the performance threshold. If you achieve 60 points you receive a 0% adjustment.
60.01.-100 Points
CMS will take the funds of those who did not meet the threshold (in red) and distribute them among those who did meet the threshold (in green). Anyone whose MIPS score is between 60.01 and 100 points will receive some portion of those funds – up to a 9% increase to their 2023 Medicare fee schedule.
85 Points and above
By scoring at least 85 points, you’ll be eligible for the Exceptional Performance bonus money (on the right). CMS has set aside an additional $500 million to distribute to anyone who scores between 85 – 100 points. This is on top of whatever portion of money you receive from those who do not participate (in red).
Note: Exceptional Performance bonus can be earned until Measurement Year 2022, Payment Year 2024
Important dates to remember
January 1, 2021 is the start date to track 365 days of Quality and Cost category measures. For the Promoting Interoperability category and the Improvement Activities category, you may start between January 1 and October 2, 2021 to track your measures for a minimum of 90 days.
The last day to submit all of your performance data is March 31, 2022.
|

.png?width=352&name=2026%20Quality%20Reporting%20Deadlines%20Guide%20(1).png)



Comments