2023 Star Ratings Calculation

CMS released the 2023 star rating for nearly all U.S. hospitals. The hospital star rating system began nearly a decade ago and is updated at least once annually. It uses a familiar system of ranking hospitals according to a star rating, with a one-star indicating poor performance and a five-star indicating excellent performance.
But while the star rating may be easy for consumers to understand, the calculation used to assess and rate hospitals is anything but simple. Today we will review how this star rating was calculated and how hospitals performed in 2023.
- Jump to: How did CMS calculate the 2023 star rating?
- Jump to: How did other hospitals perform?
Which measures did CMS use for the 2023 star rating
The star rating is made up of five categories: mortality rates, patient readmissions to the hospital, safety of care, timely and effective care, and the patient experience (as reported by patients). Within each category are a set of measures which you have submitted through your various regulatory programs or CMS has gathered through your claim submissions. Here are the measures and timeframes that were used to determine your 2023 hospital star rating.
|
Star Ratings Measure Group |
Measure ID |
Measure name |
Timeframe Used |
Measure pulled from which program(s) |
|
Mortality |
||||
|
MORT 30-AMI |
Acute Myocardial Infarction (AMI) 30-Day Mortality Rate |
July 1, 2018 - |
HVBP |
|
|
MORT 30-CABG |
Coronary Artery Bypass Graft (CABG) 30-Day Mortality Rate |
July 1, 2018 - |
HVBP |
|
|
MORT 30-COPD |
Chronic Obstructive Pulmonary Disease (COPD) 30-Day Mortality Rate |
July 1, 2018 - |
HVBP |
|
|
MORT 30-HF |
Heart Failure (HF) 30-Day Mortality Rate |
July 1, 2018 - |
HVBP |
|
|
MORT 30-PN |
Pneumonia (PN) 30-Day Mortality Rate |
July 1, 2018 - |
HVBP |
|
|
MORT 30-STK |
Acute Ischemic Stroke (STK) 30-Day Mortality Rate |
July 1, 2018 - |
IQR |
|
|
PSI 04 |
Death Rate Among Surgical Inpatients with Serious Treatable Complications |
July 1, 2019 - |
IQR |
|
|
Readmission |
||||
|
EDAC 30 AMI |
Excess Days in Acute Care after Hospitalization for Acute Myocardial Infarction |
July 1, 2018 - |
IQR |
|
|
EDAC 30 HF |
Excess Days in Acute Care after Hospitalization for Heart Failure |
July 1, 2018 - |
IQR |
|
|
EDAC- 30 PN |
Excess Days in Acute Care after Hospitalization for Pneumonia (PN) |
July 1, 2018 - |
IQR |
|
|
READM 30 CABG |
Coronary Artery Bypass Graft (CABG) 30-Day Readmission Rate |
July 1, 2018 - |
HRRP |
|
|
READM 30 COPD |
Chronic Obstructive Pulmonary Disease (COPD) 30-Day Readmission Rate |
July 1, 2018 - |
HRRP |
|
|
READM 30 HIP KNEE |
Hospital-Level 30-Day All-Cause Risk- Standardized Readmission Rate (RSRR) Following Elective Total Hip Arthroplasty (THA)/Total Knee Arthroplasty (TKA) |
July 1, 2018 - |
HRRP |
|
|
READM 30 HOSP WIDE |
HWR Hospital-Wide All-Cause Unplanned Readmission |
July 1, 2020 - |
IQR |
|
|
OP 32 |
Facility Seven-Day Risk-Standardized Hospital Visit Rate after Outpatient Colonoscopy |
January 1, 2019 - |
OQR |
|
|
OP 35 ADM |
Admissions for Patients Receiving Outpatient Chemotherapy |
January 1, 2021 - |
OQR |
|
|
OP 35 ED |
Emergency Department (ED) Visits for Patients Receiving Outpatient Chemotherapy |
January 1, 2021 - |
OQR |
|
|
OP 36 |
Hospital Visits after Hospital Outpatient Surgery |
January 1, 2021 - |
OQR |
|
|
Safety of Care |
||||
|
COMP HIP KNEE |
Hospital-Level Risk-Standardized Complication Rate (RSCR) Following Elective Primary Total Hip Arthroplasty (THA) and Total Knee Arthroplasty (TKA) |
April 1, 2018 - |
HVBP |
|
|
HAI 1 |
Central-Line Associated Bloodstream Infection (CLABSI) |
April 1, 2021 - |
HVBP, HACRP |
|
|
HAI-2 |
Catheter-Associated Urinary Tract Infection (CAUTI) |
April 1, 2021 - |
HVBP, HACRP |
|
|
HAI-3 |
Surgical Site Infection from Colon Surgery (SSI-colon) |
April 1, 2021 - |
HVBP, HACRP |
|
|
HAI-4 |
Surgical Site Infection from Abdominal Hysterectomy (SSI-abdominal hysterectomy) |
April 1, 2021 - |
HVBP, HACRP |
|
|
HAI-5 |
MRSA Bacteremia |
April 1, 2021 - |
HVBP, HACRP |
|
|
HAI-6 |
Clostridium Difficile (C.difficile) |
April 1, 2021 - |
HVBP, HACRP |
|
|
PSI 90 |
Patient Safety and Adverse Events Composite |
July 1, 2019 - |
HVBP, HACRP |
|
|
Patient Experience |
||||
|
H-COMP-1 |
Communication with Nurses |
April 1, 2021 - |
IQR, HVBP |
|
|
H-COMP-2 |
Communication with Doctors |
April 1, 2021 - |
IQR, HVBP |
|
|
H-COMP-3 |
Responsiveness of Hospital Staff |
April 1, 2021 - |
IQR, HVBP |
|
|
H-COMP-5 |
Communication About Medicines |
April 1, 2021 - |
IQR, HVBP |
|
|
Q 8 / Q 9 |
Cleanliness and Quietness of Hospital Environment |
April 1, 2021 - |
IQR, HVBP |
|
|
H-COMP-6 |
Discharge Information |
April 1, 2021 - |
IQR, HVBP |
|
|
H-COMP-7 |
Care Transition |
April 1, 2021 - |
IQR, HVBP |
|
|
Q 18 / Q 19 |
Overall Rating of Hospital & Recommend Hospital |
April 1, 2021 - |
IQR, HVBP |
|
|
Timely & Effective Care |
||||
|
HCP COVID-19 |
COVID-19 Vaccination Coverage Among HCP |
January 1, 2022 - |
IQR |
|
|
IMM-3 |
Healthcare Personnel Influenza Vaccination |
October 1, 2021 - |
IQR |
|
|
OP 10 |
Abdomen CT Use of Contrast Material |
July 1, 2020 - |
OQR |
|
|
OP 13 |
Cardiac Imaging for Preoperative Risk Assessment for Non-Cardiac Low-Risk Surgery |
July 1, 2020 - |
OQR |
|
|
OP 18b |
Median Time from ED Arrival to ED Departure for Discharged ED Patients |
April 1, 2021 - |
OQR |
|
|
OP 2 |
Fibrinolytic Therapy Received Within 30 Minutes of Emergency Department Arrival |
April 1, 2021 - |
OQR |
|
|
OP 22 |
ED-Patient Left Without Being Seen |
January 1, 2021 - |
OQR |
|
|
OP 23 |
ED-Head CT or MRI Scan Results for Acute Ischemic Stroke or Hemorrhagic Stroke who Received Head CT or MRI Scan Interpretation Within 45 Minutes of Arrival |
April 1, 2021 - |
OQR |
|
|
OP 29 |
Endoscopy/Polyp Surveillance: Appropriate Follow-up Interval for Normal Colonoscopy in Average Risk Patients |
January 1, 2021 - |
OQR |
|
|
OP 3b |
Median Time to Transfer to Another Facility for Acute Coronary Intervention |
April 1, 2021 - |
OQR |
|
|
OP 8 |
MRI Lumbar Spine for Low Back Pain |
July 1, 2020 - |
OQR |
|
|
PC 01 |
Elective Delivery Prior to 39 Completed Weeks Gestation: Percentage of Babies Electively Delivered Prior to 39 Completed Weeks Gestation |
April 1, 2021 - |
IQR |
|
|
SEP 1 |
Severe Sepsis and Septic Shock |
April 1, 2021 - |
IQR, HVBP |
|
There were two measures changes as compared to the previous star rating assessment. CMS retired OP-33 from the Timely and Effective Care category as of January 2022 and it is no longer part of your star ratings calculation. CMS added the HCP COVID-19 measures to the Timely Effective Care category for star rating calculation. Also, for the first time, the star rating included VA hospitals.
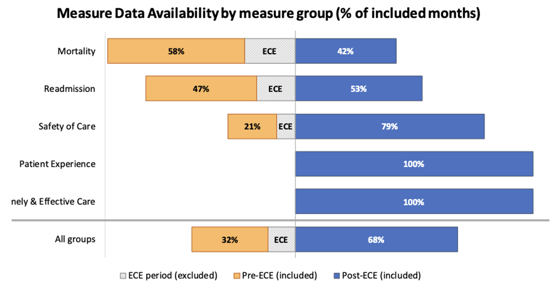
Additionally, CMS did modify some of the above timeframes based on COVID-19 impact to hospital performance. There were 15 measures (found in either the Mortality or Readmission category) that would normally include Q1 and Q2 2020 data but because of the pandemic they were excluded. Because of these changes, CMS calculated your star ratings using the majority of data (68%) to be reflective of your care after June 30, 2020.
How Did CMS Calculate the 2023 Hospital Star Rating?
The star rating calculation was simplified in 2021 and now is calculated in 10 steps.
STEP 1: Hospitals submit data to CMS quality programs
You, as a hospital, go about your business of submitting measures to the CMS quality programs: Hospital IQR, OQR, Readmission Reduction, HAC Reduction and HVBP programs. See programs referenced above. Sometimes you submit the measure (like SEP-1) and sometimes CMS collects the data from claims files.
STEP 2: CMS identifies which measures and timeframes to use
CMS selects which measures they will use to make the star rating score. The measures used in the 2023 star rating are listed above.
STEP 3: CMS standardizes the measure scores
CMS takes your hospital’s performance on those CMS-selected measures and standardizes the measure score so it makes sense in the overall equation. Think about an inverse measure where lower scores are better. You wouldn’t want that score to count against a total score, so they standardize all measure scores. This method of standardizing is called Z-scoring.
Understanding Z-scoring
A Z score is statistical technique. It’s a standard deviation score which shows the amount of variation in a dataset. For the star rating, Z-scores were produced by subtracting the national mean score from each hospital’s measure score and dividing that by the standard deviation across hospitals. Standard deviation is a number that measures how far data values are from their average.
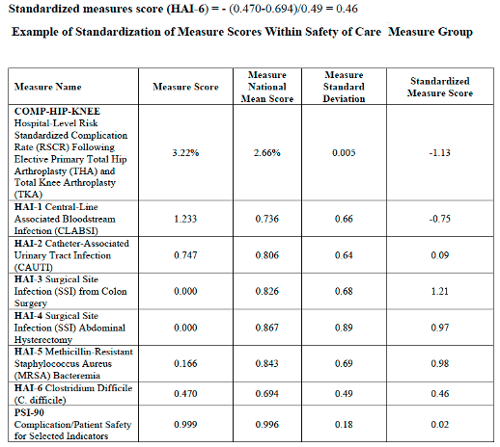
In addition to that, CMS changed the direction of all inverse measures to reflect better performance for those lower scores.
STEP 4: Measures are grouped
The measures are put into groups based on the category. The five measures groups are:
- Mortality
- Safety of Care
- Readmissions
- Patient Experience
- Timely and Effective Care
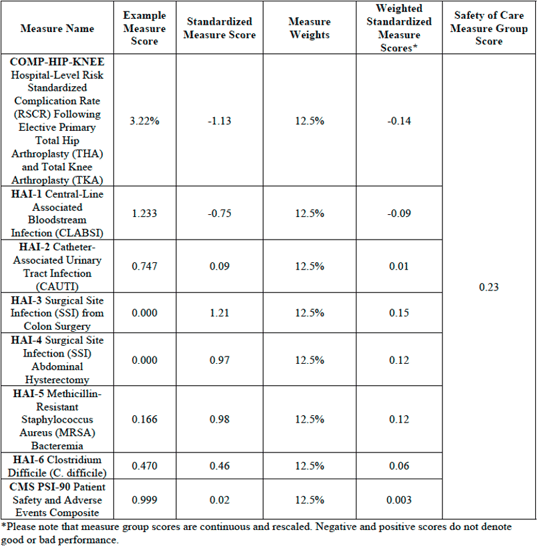
STEP 5: CMS calculates the measure group score using a simple average
In each measure group, CMS will calculate a simple average to determine a measure group score. A simple average takes the sum of measures with equal weights and divides by the number of measures a hospital reports.
For example:
There are 8 measures in the Safety of Care category.
100 divided by 8 is 12.5 so each of the 8 measures in this category would be worth 12.5% of the overall Safety of Care category score.
100% / 8 measures = 12.5%
Measure group score (based on example above) =
[(-1.13*0.125) + (-0.75*0.125) + (0.09*0.125) + (1.21*0.125) + (0.97*0.125) + (0.98*0.125) + (0.46*0.125) + (0.02*0.125)] = 0.23
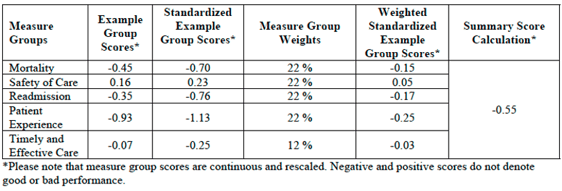
STEP 6: CMS applies a weight to each group score
Not all categories are weighted evenly. A weight is applied to that measure group score. Your final score is calculated according to the weight of the category. The weights for the five categories are as follows:
- Mortality = 22% weight
- Safety of Care = 22% weight
- Readmissions = 22% weight
- Patient Experience = 22% weight
- Timely and Effective Care = 12% weight
For Example:
Summary score = [(-0.70*0.22) + (0.23*0.22) + (-0.76*0.22) + (-1.13*0.22) + (-0.25*0.12)] = -0.55
STEP 7: Hospitals are excluded, or their score is re-weighted depending on the number of measures submitted
Not all hospitals submit (or have enough claims) to qualify for every measure in all five categories. A hospital must report at least three measure groups with at least three measures in each group, (must include groups Mortality or Safety of Care) in order to receive a star rating. Once the minimum measure and measure group thresholds are met, any additional measures a hospital reports would be included in the star rating calculation.
Let’s say you met the minimum threshold, but you didn’t have any measures that were able to be calculated in the Timely and Effective Care category. That measure group is subtracted from the total.
For Example:
100 (100-12=88)
Mortality weight: 22/88 = 25%
Safety of Care weight: 22/88 = 25%
Readmission weight: 22/88 = 25%
Patient Experience weight: 22/88 = 25%
Example of Reweighting for a Hospital Which Does Not Report Timely and Effective Care Measure Group
![ReweightingNoTimelyCareScoreStarRating[88]](https://blog.medisolv.com/hs-fs/hubfs/ReweightingNoTimelyCareScoreStarRating%5B88%5D.png?width=540&height=233&name=ReweightingNoTimelyCareScoreStarRating%5B88%5D.png)
STEP 8: Hospitals are put into one of three peer groups based on the number of measures they submitted
Hospitals are put into one of three peer groups depending on how many measures they submit or are calculated. CMS believes that by grouping hospitals by how many measure groups they report, this will help capture key differences between hospitals like size, patient volume, case mix and service mix. Larger hospitals, for example, generally submit the most measures and smaller hospitals submit the fewest.
The three peer groups are:
- Five measure groups submitted
- Four measure groups submitted
- Three measure groups submitted
STEP 9: Within the peer groups, scores are split into 5 groups using the k-means clustering method
Within the peer grouping, scores are split into five groups using the k-means clustering method. Essentially the k-means clustering is an algorithm method which aims to make hospital scores results within a cluster more similar to each other than to a different cluster.
STEP 10: whichever group your score puts you in becomes your star rating
Whichever k-means clustering group your score puts you in becomes your star rating.
Note: Since hospitals in a peer group are being compared only to each other that means hospitals with the same score, but a different peer group, could receive different star ratings.
How Did Other Hospitals Perform?
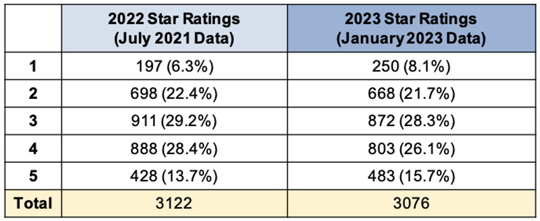
There were 3,076 hospitals who received a star rating in 2023 as compared to 3,122 hospitals in 2022.
This year:
- 250 (8%) got 1 star
- 668 (22%) got 2 stars
- 872 (28%) got 3 Stars
- 803 (26%) got 4 stars
- 483 (16%) got 5 stars
The distribution of star ratings is similar to the distribution in 2022.
Medisolv had 117 of the 438 5-star hospitals. Congratulations to all of our 5-star hospitals listed below.
How to Improve Your Star Rating
If you made it this far down in the article, congratulations; you are one step closer to improving your star rating. Simply by understanding how the star rating is calculated and what timeframes they consider will help you to understand what to focus on.
It comes down to ensuring you are doing everything you can to improve your performance across the major regulatory programs I mentioned in Step 1: Hospital IQR, OQR, Readmission Reduction, HAC Reduction and HVBP programs.
These measures are used for more than just star rating calculation, they are publicly reported on Care Compare. The public facing website contains not just the measures from your star ratings, but a whole host of additional measures submitted in those regulatory programs. Furthermore, the Care Compare measures are used, at least in part, for almost every public hospital ranking program today. Some popular programs are the U.S. World and News Reports for Best Hospitals and the Leapfrog Hospital Safety Grades which assigns letter grades for all hospitals.
The number of stars and your public performance may influence the credibility, efficiency, culture, and financial state of your organization.
Congratulations to Medisolv's 5-Star Hospitals:
| Mayo Clinic Hospital - Arizona | Buffalo Hospital |
| UC San Diego Medical Center | Mayo Clinic Health System - Mankato |
| Sharp Grossmont Hospital | M Health Fairview Woodwinds Hospital |
| UCLA Health - Santa Monica Medical Center | Baptist Memorial Hospital - Union County |
| Ronald Reagan UCLA Medical Center | Baptist Memorial Hospital - Leake |
| Goleta Valley Cottage Hospital | Missouri Baptist Medical Center |
| Community Memorial Hospital - Ventura | Saint Lukes Hospital of Kansas City |
| Santa Barbara Cottage Hospital | Barnes-Jewish St Peters Hospital |
| University of California San Francisco Health System | Saint Lukes East Hospital |
| UCSF Helen Diller Medical Center at Parnassus Heights | Progress West Hospital |
| Keck Hospital of USC | Hedrick Medical Center |
| Whittier Hospital Medical Center | Cox Monett Hospital |
| Greater El Monte Community Hospital | Bryan East Campus |
| UCHealth Poudre Valley Hospital | Bellevue Medical Center |
| UCHealth University of Colorado Hospital | Exeter Hospital |
| UCHealth Medical Center of the Rockies | Hackensack University Medical Center |
| MidState Medical Center | Morristown Medical Center |
| Lee Memorial Hospital | NewYork-Presbyterian Queens |
| Baptist Medical Center Nassau | NewYork-Presbyterian Weill Cornell Medical Center |
| Mayo Clinic Hospital - Florida | Tisch Hospital |
| St Lukes Boise Medical Center | NYU Langone Health |
| Evanston Hospital (AKA NorthShore Evanston Hospital) | Duke University Hospital |
| Rush Oak Park Hospital | Watauga Medical Center |
| Northwestern Medicine McHenry Hospital | UNC Medical Center |
| Rush University Medical Center | Duke Raleigh Hospital |
| Carle BroMenn Medical Center | UNC Rex Hospital |
| Northwestern Medicine Lake Forest Hospital | Wake Forest Baptist Health - Davie Medical Center |
| Northwestern Medicine Delnor Hospital | Novant Health Mint Hill Medical Center |
| Northwestern Medicine Central DuPage Hospital | The Outer Banks Hospital |
| Northwestern Memorial Hospital | Essentia Health - Fargo |
| Northwestern Medicine Kishwaukee Hospital | OhioHealth OBleness Hospital |
| IU Health North Hospital | Wooster Community Hospital |
| Boone County Hospital | OhioHealth Dublin Methodist Hospital |
| The University of Kansas Hospital | Surgical Hospital at Southwoods (AKA Southwoods Health) |
| Saint Lukes South Hospital | INTEGRIS Health Grove Hospital |
| St Tammany Health System | OHSU Hospital - Portland (AKA OHSU Hospital - Marquam Hill Campus) |
| UM St Joseph Medical Center | Bryn Mawr Hospital |
| Mount Auburn Hospital | Doylestown Hospital (AKA Doylestown Health) |
| Massachusetts General Hospital | South County Hospital |
| Emerson Hospital | Miriam Hospital |
| Milford Regional Medical Center | Prisma Health Patewood Hospital |
| Winchester Hospital | Sanford USD Medical Center |
| Beth Israel Deaconess Hospital - Milton | North Texas Medical Center |
| Brigham and Womens Hospital | Methodist Hospital Hill Country |
| Lahey Hospital & Medical Center - Burlington | Memorial Hermann Sugar Land Hospital |
| Spectrum Health Zeeland Community Hospital | University of Utah Hospital |
| MyMichigan Medical Center Alpena | The University of Vermont Medical Center |
| Spectrum Health Butterworth Hospital | Southwestern Vermont Medical Center |
| Spectrum Meijer Heart Center | Porter Medical Center |
| University Hospital | University Hospital |
| UP Health System - Portage Main Campus | Carilion Giles Community Hospital |
| Sparrow Eaton Hospital | Mayo Clinic Health System - Franciscan Healthcare La Crosse |
| Spectrum Health Gerber Memorial | Mayo Clinic Health System - Eau Claire |
| Essentia Health - St Marys Medical Center | Howard Young Medical Center |
| Mayo Clinic Hospital - Saint Marys Campus | University Hospital |
| Essentia Health - Duluth | Mayo Clinic Health System - Northland in Barron |
| Cambridge Medical Center | Mayo Clinic Health System - Red Cedar in Menomonie |
| Mayo Clinic Health System - Albert Lea | ThedaCare Medical Center - Berlin |
| Abbott Northwestern Hospital |
Sources:
i. https://public-inspection.federalregister.gov/2020-26819.pdf
ii. https://www.aha.org/system/files/media/file/2020/12/cms-issues-hospital-outpatient-asc-final-rule-including-maintenance-340b-cuts-bulletin-12-3-20.pdf
iii. https://www.sheppardhealthlaw.com/2020/12/articles/centers-for-medicare-and-medicaid-services-cms/new-criteria-hospital-quality-star-rating/
iv. https://qualitynet.cms.gov/inpatient/public-reporting/overall-ratings/data-collection
|
Ready to Improve Your CMS Hospital Star Rating? Understanding your score is just the first step. Improving it requires clarity, strategy, and the right tools. Start with insight. Medisolv’s Free Hospital Star Rating Assessment Tool gives you an instant breakdown of your CMS calculation. Simply upload your Hospital Specific Report (HSR) and receive:
Try it free: Ready for deeper intelligence? Watch the Analyzer demo on-demand and see how it works in action. |



.png?width=352&name=2026%20Quality%20Reporting%20Deadlines%20Guide%20(1).png)

Comments