2025 Star Ratings Calculation
.png?width=900&height=600&name=BlogImage_2025%20Star%20Ratings%20(1).png)
CMS released the 2025 star rating for nearly all U.S. hospitals. The hospital star rating system began nearly a decade ago and is updated at least once annually. It uses a familiar system of ranking hospitals according to a star rating, with a one-star indicating poor performance and a five-star indicating excellent performance.
But while the star rating may be easy for consumers to understand, the calculation used to assess and rate hospitals is anything but simple. Today we will review how this star rating was calculated and how hospitals performed in 2025.
- Jump to: How did other hospitals perform?
- Jump to: Which measures did CMS use?
Star Ratings Overview & Updates
The star rating is made up of five categories: mortality rates, patient readmissions to the hospital, safety of care, timely and effective care, and the patient experience (as reported by patients). Within each category are a set of measures which you have submitted through your various regulatory programs or CMS has gathered through your claim submissions. At the bottom of this article is the full list of the measures (and the timeframes) CMS used to determine your 2025 star rating.
This year, the major update is that CMS utilized an eCQM for the first time to determine a Hospital Star Rating performance. Woah! Are there more to come? My bet is yes. And I'm going to guess it will be the maternal measures (PC 02, PC 07). Why? Because PC 01 was retired and PC 02 & PC 07 are now eligible for inclusion.
Additionally, CMS did modify some of the timeframes based on COVID-19's impact to hospital performance. There were some measures that would normally include Q1 and Q2 2020 data, but because of the pandemic they were excluded. Because of these changes, CMS calculated your star ratings using data reflecting your care after June 30th, 2020.
How Did CMS Calculate the 2025 Hospital Star Rating?
The star rating calculation was simplified in 2021 and now is calculated in 11 steps.
STEP 1: Hospitals submit data to CMS quality programs
Your hospital submits measures to the CMS quality programs such as the Hospital IQR and OQR programs. Your measures are used to assess your performance on the value programs such as the Hospital-Acquired Condition Reduction, Readmission Reduction, and Value Based Purchasing programs. Sometimes you submit the measure (like SEP-1) or the Safe Use of Opioids eCQM and sometimes CMS collects the data from claims files.
STEP 2: CMS identifies which measures and timeframes to use
CMS selects which measures they will use to make the star rating score. The measures used in the 2025 star rating are listed at the bottom of this article.
STEP 3: CMS standardizes the measure scores
CMS takes your hospital’s performance on those CMS-selected measures and standardizes the measure score, so it makes sense in the overall equation. Think about an inverse measure where lower scores are better. You wouldn’t want that score to count against a total score, so they standardize all measure scores. This method of standardizing is called Z-scoring.
Understanding Z-scoring
A Z score is a statistical technique. It’s a standard deviation score, which shows the amount of variation in a dataset. For the star rating, Z-scores were produced by subtracting the national mean score from each hospital’s measure score and dividing that by the standard deviation across hospitals. Standard deviation is a number that measures how far data values are from their average.

In addition to that, CMS changed the direction of all inverse measures to reflect better performance for those with lower scores. To do that, any inverse measures are multiplied by -1 before dividing by the standard deviation. For instance, HAI-6 = (0.47-0.694) * -1 / 0.49 = 0.46. Also, note, if you just plug this formula into a calculator it will be wrong. That's because your results are calculated out to the 16th decimal, so these tiny little fractions of numbers make a big difference in the outcome of the measure. The complete numbers can be found in your Hospital Specific Report (HSR) report.
STEP 4: Measures are grouped
The measures are put into groups based on the category. The five measure groups are:
- Mortality
- Readmissions
- Safety of Care
- Patient Experience
- Timely and Effective Care
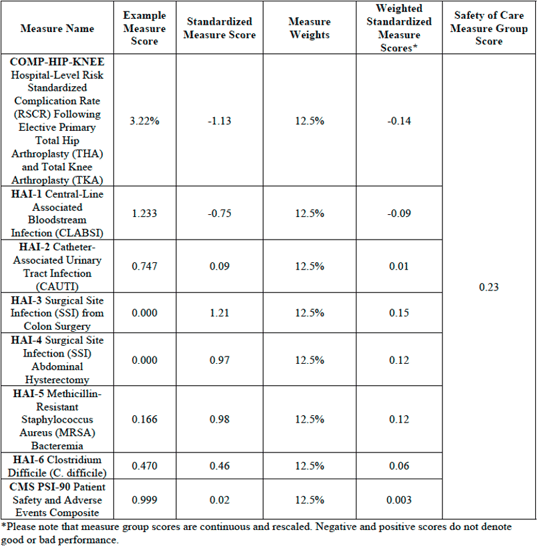
STEP 5: CMS calculates the measure group score using a simple average
For each measure group, CMS will calculate a simple average to determine a measure group score. A simple average takes the sum of measures with equal weights and divides it by the number of measures a hospital reports.
For example:
There are 8 measures in the Safety of Care category.
100 divided by 8 is 12.5 so each of the 8 measures in this category would be worth 12.5% of the overall Safety of Care category score.
100% / 8 measures = 12.5%
Measure group score (based on example below) =
[(-1.13*0.125) + (-0.75*0.125) + (0.09*0.125) + (1.21*0.125) + (0.97*0.125) + (0.98*0.125) + (0.46*0.125) + (0.02*0.125)] = 0.23
STEP 6: CMS calculates your hospital's standardized score for the Measure Group
In Step 3, CMS used a formula to standardize each measure within the measure group. In this step, they do the same calculation using the overall measure group score.
| Measure Group Name | Group Measure Score | National Group Measure Score | National Standard Deviation | Standardized Measure Group Score |
| Safety of Care | 0.46 | -0.02 | 0.78 | 0.61 |
Safety of Care = (0.46 - -0.02) / 0.78 = 0.61
Remember, you've got to have the full fractions to make these calculations work!
STEP 7: CMS applies a weight to each group's score
Not all categories are weighted equally. A weight is applied to that measure group score. Your final score is calculated according to the weight of the category. The weights for the five categories are as follows:
- Mortality = 22% weight
- Safety of Care = 22% weight
- Readmissions = 22% weight
- Patient Experience = 22% weight
- Timely and Effective Care = 12% weight
For Example:
Summary score = [(-0.70*0.22) + (0.23*0.22) + (-0.76*0.22) + (-1.13*0.22) + (-0.25*0.12)] = -0.55
STEP 8: Hospitals are excluded, or their score is re-weighted depending on the number of measures submitted
Not all hospitals submit (or have enough claims) to qualify for every measure in all five categories. A hospital must report at least three measure groups with at least three measures in each group (must include groups, Mortality or Safety of Care) to receive a star rating. Once the minimum measure and measure group thresholds are met, any additional measures a hospital reports will be included in the star rating calculation.
Let’s say you met the minimum threshold, but you didn’t have any measures that could be calculated in the Timely and Effective Care category. That measure group is subtracted from the total.
For Example:
100 (100-12=88)
Mortality weight: 22/88 = 25%
Safety of Care weight: 22/88 = 25%
Readmission weight: 22/88 = 25%
Patient Experience weight: 22/88 = 25%
Example of Reweighting for a Hospital Which Does Not Report Timely and Effective Care Measure Group
![ReweightingNoTimelyCareScoreStarRating[88]](https://blog.medisolv.com/hs-fs/hubfs/ReweightingNoTimelyCareScoreStarRating%5B88%5D.png?width=540&height=233&name=ReweightingNoTimelyCareScoreStarRating%5B88%5D.png)
STEP 9: Hospitals are put into one of three peer groups based on the number of measures they submitted
Hospitals are put into one of three peer groups depending on how many measures they submit or are calculated. CMS believes that by grouping hospitals by how many measure groups they report, this will help capture key differences between hospitals like size, patient volume, case mix, and service mix. Larger hospitals, for example, generally submit the most measures and smaller hospitals submit the fewest.
The three peer groups are:
- Five measure groups submitted
- Four measure groups submitted
- Three measure groups submitted
STEP 10: Within the peer groups, scores are split into 5 groups using the k-means clustering method
Within peer grouping, scores are split into five groups using the k-means clustering method. Essentially, the k-means clustering is an algorithm method which aims to make hospital scores results within a cluster more similar to each other than to a different cluster.
STEP 11: Whichever group your score puts you in becomes your star rating
Whichever k-means clustering group your score puts you in becomes your star rating.
Note: Since hospitals in a peer group are being compared only to each other, that means hospitals with the same score, but a different peer group, could receive different star ratings.
| July 2025 | |||
| Overall Star Rating | 3-measure groups (n=141) | 4-measure groups (n=515) | 5-measure groups (n=2,235) |
| 1 Star | -3.351 to -1.638 | -1.654 to -0.565 | -2.468 to -0.669 |
| 2 Star | -1.343 to -0.641 | -0.543 to -0.035 | -0.666 to -0.277 |
| 3 Star | -0.597 to -0.050 | -0.033 to 0.411 | -0.276 to 0.073 |
| 4 Star | -0.036 to 0.423 | 0.417 to 0.911 | 0.074 to 0.459 |
| 5 Star | 0.476 to 1.298 | 0.934 to 2.064 | 0.460 to 1.618 |
How Did Other Hospitals Perform?
There were 2,891 hospitals that received a star rating in 2025.
This year:
- 233 (8%) got 1 star
- 663 (23%) got 2 stars
- 942 (33%) got 3 Stars
- 762 (27%) got 4 stars
- 291 (10%) got 5 stars
How to Improve Your Star Rating
If you made it this far down in the article, congratulations, you are one step closer to improving your star rating. Simply by understanding how star ratings are calculated and what timeframes they consider will help you to understand what to focus on.
It's about making sure you're doing everything you can to improve your performance in the main regulatory programs I mentioned in Step 1: Hospital IQR, OQR, HRRP, HACRP, and HVBP programs.
These measures are used for more than just star rating calculations; they are publicly reported on Care Compare. The public-facing website contains not just the measures from your star ratings, but a whole host of additional measures submitted in those regulatory programs. Furthermore, the Care Compare measures are used, at least in part, for almost every public hospital ranking program today. Some popular programs are the U.S. World and News Reports for Best Hospitals and the Leapfrog Hospital Safety Grades, which assigns letter grades for all hospitals.
The number of stars and your public performance may influence the credibility, efficiency, culture, and financial state of your organization.
Medisolv provides Star Ratings Advisory Services. If you'd like to have your 2025 Star Ratings HSR evaluated and learn how our clinical experts can help your team excel in Star Ratings, reach out to us today.
Which Measures Did CMS Use for the 2025 Star Rating?
| Measure ID | Measure Name | Measure Reporting Period |
|
| Mortality | |||
| MORT-30-AMI | Acute Myocardial Infarction (AMI) 30-Day Mortality Rate | July 1, 2020 - June 30, 2023 | |
| MORT-30-CABG | Coronary Artery Bypass Graft (CABG) 30-Day Mortality Rate | July 1, 2020 - June 30, 2023 | |
| MORT-30-COPD | Chronic Obstructive Pulmonary Disease (COPD) 30-Day Mortality Rate | July 1, 2020 - June 30, 2023 | |
| MORT-30-HF | Heart Failure (HF) 30-Day Mortality Rate | July 1, 2020 - June 30, 2023 | |
| MORT-30-PN | Pneumonia (PN) 30-Day Mortality Rate | July 1, 2020 - June 30, 2023 | |
| MORT-30-STK | Acute Ischemic Stroke (STK) 30-Day Mortality Rate | July 1, 2020 - June 30, 2023 | |
| PSI 04 | Death Rate Among Surgical Inpatients with Serious Treatable Complications | July 1, 2021 - June 30, 2023 | |
| Readmission | |||
| EDAC-30-AMI | Excess Days in Acute Care after Hospitalization for Acute Myocardial Infarction | July 1, 2020 - June 30, 2023 | |
| EDAC-30-HF | Excess Days in Acute Care after Hospitalization for Heart Failure | July 1, 2020 - June 30, 2023 | |
| EDAC-30-PN | Excess Days in Acute Care after Hospitalization for Pneumonia (PN) | July 1, 2020 - June 30, 2023 | |
| READM-30-CABG | Coronary Artery Bypass Graft (CABG) 30-Day Readmission Rate | July 1, 2020 - June 30, 2023 | |
| READM-30-COPD | Chronic Obstructive Pulmonary Disease (COPD) 30-Day Readmission Rate | July 1, 2020 - June 30, 2023 | |
| READM-30-Hip-Knee | Hospital-Level 30-Day All-Cause Risk- Standardized Readmission Rate (RSRR) Following Elective Total Hip Arthroplasty (THA)/Total Knee Arthroplasty (TKA) | July 1, 2020 - June 30, 2023 | |
| READM-30-HOSP-WIDE | HWR Hospital-Wide All-Cause Unplanned Readmission | July 1, 2022 - June 30, 2023 | |
| OP-32 | Facility Seven-Day Risk-Standardized Hospital Visit Rate after Outpatient Colonoscopy | July 1, 2020 - December 31, 2022 | |
| OP-35 ADM | Admissions for Patients Receiving Outpatient Chemotherapy | January 1, 2022 - December 31, 2022 | |
| OP-35 ED | Emergency Department (ED) Visits for Patients Receiving Outpatient Chemotherapy | January 1, 2022 - December 31, 2022 | |
| OP-36 | Hospital Visits after Hospital Outpatient Surgery | January 1, 2022 - December 31, 2022 | |
| Safety of Care | |||
| COMP-HIP-KNEE | Hospital-Level Risk-Standardized Complication Rate (RSCR) Following Elective Primary Total Hip Arthroplasty (THA) and Total Knee Arthroplasty (TKA) | July 1, 2020 - March 31, 2023 | |
| HAI-1 | Central-Line Associated Bloodstream Infection (CLABSI) | January 1, 2023 - December 31, 2023 | |
| HAI-2 | Catheter-Associated Urinary Tract Infection (CAUTI) | January 1, 2023 - December 31, 2023 | |
| HAI-3 | Surgical Site Infection from Colon Surgery (SSI-colon) | January 1, 2023 - December 31, 2023 | |
| HAI-4 | Surgical Site Infection from Abdominal Hysterectomy (SSI-abdominal hysterectomy) | January 1, 2023 - December 31, 2023 | |
| HAI-5 | MRSA Bacteremia | January 1, 2023 - December 31, 2023 | |
| HAI-6 | Clostridium Difficile (C.difficile) | January 1, 2023 - December 31, 2023 | |
| PSI 90 | Patient Safety and Adverse Events Composite | July 1, 2021 - June 30, 2023 | |
| Patient Experience | |||
| H-COMP-1 | Communication with Nurses | January 1, 2023 - December 31, 2023 | |
| H-COMP-2 | Communication with Doctors | January 1, 2023 - December 31, 2023 | |
| H-COMP-3 | Responsiveness of Hospital Staff | January 1, 2023 - December 31, 2023 | |
| H-COMP-5 | Communication About Medicines | January 1, 2023 - December 31, 2023 | |
| H-COMP-6 | Discharge Information | January 1, 2023 - December 31, 2023 | |
| H-COMP-7 | Care Transition | January 1, 2023 - December 31, 2023 | |
| H-CLEAN-HSP / H-QUIET-HSP | Cleanliness and Quietness of Hospital Environment | January 1, 2023 - December 31, 2023 | |
| H-HSP-RATING / H-RECMND | Overall Rating of Hospital | January 1, 2023 - December 31, 2023 | |
| Timely & Effective Care | |||
| HCP COVID-19 | COVID-19 Vaccination Coverage Among HCP | October 1, 2023 - December 31, 2023 | |
| IMM-3 | Healthcare Personnel Influenza Vaccination | October 1, 2023 - March 31, 2024 | |
| OP-10 | Abdomen CT Use of Contrast Material | July 1, 2022 - June 30, 2023 | |
| OP-13 | Cardiac Imaging for Preoperative Risk Assessment for Non-Cardiac Low-Risk Surgery | July 1, 2022 - June 30, 2023 | |
| OP-18b | Median Time from ED Arrival to ED Departure for Discharged ED Patients | January 1, 2023 - December 31, 2023 | |
| OP-22 | ED-Patient Left Without Being Seen | January 1, 2022 - December 31, 2022 | |
| OP-23 | ED-Head CT or MRI Scan Results for Acute Ischemic Stroke or Hemorrhagic Stroke who Received Head CT or MRI Scan Interpretation Within 45 Minutes of Arrival | January 1, 2023 - December 31, 2023 | |
| OP-29 | Endoscopy/Polyp Surveillance: Appropriate Follow-up Interval for Normal Colonoscopy in Average Risk Patients | January 1, 2022 - December 31, 2022 | |
| OP-8 | MRI Lumbar Spine for Low Back Pain | July 1, 2022 - June 30, 2023 | |
| PC-01 | Elective Delivery Prior to 39 Completed Weeks Gestation: Percentage of Babies Electively Delivered Prior to 39 Completed Weeks Gestation | January 1, 2023 - December 31, 2023 | |
| Safe Use of Opioids | Safe use of opioids - concurrent prescribing | January 1, 2023 - December 31, 2023 | |
| SEP-1 | Severe Sepsis and Septic Shock | January 1, 2023 - December 31, 2023 | |
|
Ready to Improve Your CMS Hospital Star Rating? Understanding your score is just the first step. Improving it requires clarity, strategy, and the right tools. Start with insight. Medisolv’s Free Hospital Star Rating Assessment Tool gives you an instant breakdown of your CMS calculation. Simply upload your Hospital Specific Report (HSR) and receive:
Try it free: Ready for deeper intelligence? Watch the Analyzer demo on-demand and see how it works in action. |
Sources:
- https://public-inspection.federalregister.gov/2020-26819.pdf
- https://www.aha.org/system/files/media/file/2020/12/cms-issues-hospital-outpatient-asc-final-rule-including-maintenance-340b-cuts-bulletin-12-3-20.pdf
- https://www.sheppardhealthlaw.com/2020/12/articles/centers-for-medicare-and-medicaid-services-cms/new-criteria-hospital-quality-star-rating/
- https://qualitynet.cms.gov/inpatient/public-reporting/overall-ratings/data-collection
- https://www.qualityreportingcenter.com/globalassets/iqr2024events/iqr042524/2024-npc-slides_for-cms-clearance_updated_4.17.24_508.pdf



.png?width=352&name=2026%20Quality%20Reporting%20Deadlines%20Guide%20(1).png)

Comments