A Guide to CMS's New Health Equity Measure
There has been a lot of talk around health equity. Now we are finally getting real action from CMS in the form of a new structural measure: the Hospital Commitment to Health Equity measure (HCHE).
Officially adopted in August as part of CMS's IPPS Final Rule for CY2023, the Hospital Commitment to Health Equity measure requires you to attest to whether or not your organization is reviewing and prioritizing equitable care. The measure will be mandatory as part of your 2023 Inpatient Quality Reporting (IQR) requirements.
Sidebar: CMS is also introducing two equity-focused process measures in 2023: Screening for Social Drivers of Health (SDOH-01) and Screen Positive Rate for Social Drivers of Health (SDOH-02). Although you can begin tracking them in 2023, they won’t be required until 2024. Stay tuned for more Medisolv guidance on those measures in the near future!
For now, let’s keep things simple(..ish) by focusing just on the Hospital Commitment to Health Equity measure. What is it? How is it being measured? And what do you need to do now to ensure a successful first year? Let’s get started.
The Goal of the Measure
The goal of the Hospital Commitment to Health Equity measure is not to track how equitable your care is; it’s simply to understand if your organization has made health equity a strategic priority (and to motivate you to get moving if you haven’t). That’s because CMS understands that health equity isn’t something that can happen overnight. The first thing any hospital needs is an organizational commitment to cultural change and leadership accountability.
There is data to back this up. In developing the measure, CMS reviewed 112 published studies regarding general quality improvement and found that “strong leadership that prioritized safety, quality, and the setting of clear guidance with measurable goals for improvement resulted in a high-performing hospital with better patient outcomes.” CMS posits that if strong leadership can lead a hospital to higher quality care, it can also lead a hospital to more equitable care.
How the Measure is Scored
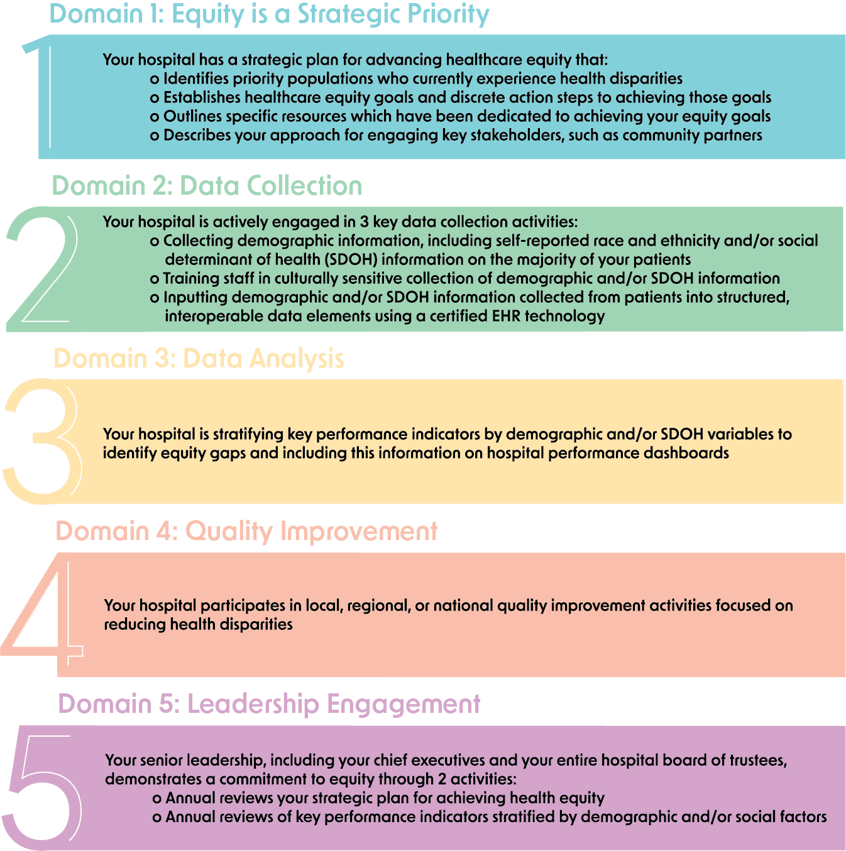
The Hospital Commitment to Health Equity measure is broken down into 5 domains, which we’ve outlined for you below. Each of the 5 domains is worth 1 point for a total of 5 possible points. However, in order to earn each domain’s point, you must affirmatively attest to ALL of the elements within that domain. As an added motivator, CMS has indicated that scores for this measure will be publicly reported.
The 5 Domains You Need to Track
Let’s now look at the Hospital Commitment to Health Equity measure’s 5 domains, broken down into simple terms. Remember, you need to be able to say “yes” to ALL of the elements (bullet points) under each domain in order to earn that domain’s point.
4 Questions To Ask Your Team Now
As you can see from the 5 domains, having a well thought-out data strategy is fundamental to your success with the Hospital Commitment to Health Equity measure. Gather your quality improvement, IT, and DEI teams and make sure you can answer these 4 questions:
-
Are we capturing the right data? As domain 2 indicates, you need to be collecting, at a minimum, self-reported race and ethnicity data or SDOH data on your patient population.
-
Are we stratifying our data correctly? The patient care metrics that your hospital tracks need to be stratified by demographic and/or SDOH data if you want to have success with this and future health equity measures and (more importantly) begin to identify disparities in your care.
-
Do we have formal processes in place for evaluating our data? Your stratified data needs to be readily available on your hospital’s quality improvement dashboard, but the job of monitoring this data shouldn’t rest solely on the shoulders of your quality improvement or DEI teams. Your C-suite and your board must be conducting, at minimum, an annual review of the data and your strategic plan.
-
Is our leadership doing more than data reviews? This takes us back to domain 1. You can collect and stratify data all day long, but if leadership hasn’t signed off on a strategic plan—and allocated the right resources—to make health equity a hospital-wide priority, your success with health equity measures will be in jeopardy.
2 Tools That Can Make Your Life Easier
As health equity efforts gain momentum in hospitals nationwide, you can expect to see a cottage industry of products and services springing up to support you. For now, here are two tools that we think are immediately worth a closer look:
-
Quality management software that’s ready for the health equity movement: This may sound like shameless self-promotion but we mean it in earnest. If you have a current quality management vendor, ask them now how they can help you collect and stratify your demographic and SDOH data to meet today’s and tomorrow’s health equity metrics.
If you don’t have a vendor and are shopping around—ask the same exact question. We are only in the dawn of health equity measurement. Any quality management solutions you invest in now should be prepared for the revolution that's just ahead.
-
The American Hospital Association’s Health Equity Roadmap: The AHA’s Health Equity Roadmap is a 100% free framework to help hospitals like yours create and execute a plan for becoming a more equitable and inclusive organization.
The Roadmap includes 3 components: 1) a Health Equity Transformation Assessment you can take to establish your hospital’s current baseline and identify realistic goals, 2) a Health Equity Transformation Model that gives you technical and operational guidelines for improvement in 6 key “levers” or areas for transformation, and 3) a Health Equity Action Library filled with practical toolkits you can use for each “lever” of transformation.
Get Help Now—Before CMS’s Health Equity Measures Hit
If you don’t want to navigate the new Hospital Commitment to Health Equity measure alone, Medisolv can help. Our platform—combined with the expertise of our clinical quality advisors—gives you the power to stratify your data to meet 2023’s requirements and beyond.
Schedule a 1:1 session to get started, or browse our Education Center to learn more about what’s next on the health equity and quality improvement horizon:
Medisolv Can HelpAlong with award-winning software, each client receives a dedicated Clinical Quality Advisor that helps you with your technical and clinical needs. We consistently hear from our clients that the biggest differentiator between Medisolv and other vendors is the level of one-of-one support. Especially if you use an EHR vendor right now, you’ll notice a huge difference.
|






Comments