How to Prepare for CMS’s New Sepsis Requirements
Everyone’s favorite core measure, the Severe Sepsis and Septic Shock: Management Bundle (SEP-1), has been added to CMS’s Hospital Value Based Purchasing (HVBP) Program in FY 2026. That’s according to the FY 2024 IPPS Final Rule that CMS released August 2023.
NEW Medisolv Survey Shows Feelings on CMS Sepsis Requirements are...Complicated.
It’s no secret that the Severe Sepsis and Septic Shock measure has become one of clinicians’ and quality leaders’ least favorite requirements since it was first introduced in the IQR program in 2015. It is notoriously labor intensive and complex to measure. And many clinicians feel that it’s too rigid in its treatment protocol. Some even suggest that, in standardizing the quick administration of antibiotics, the SEP-1 protocol actually contributes to the growing issue of antibiotic resistance.
To gauge the current climate around SEP-1, Medisolv surveyed more than 250 healthcare quality leaders nationwide. What we found a very mixed bag of feelings:
- 65% of quality leaders felt that SEP-1 “does” or “absolutely does” help them identify the places they need to focus on to improve patient care.
- Yet the majority of quality leaders surveyed (43%) are “opposed” or “adamantly opposed” to adding the sepsis requirements to the HVBP program. Only 25% are “in favor” or “adamantly in favor” of the move.
Why the Severe Sepsis and Septic Shock Measure – and Why Now?
Despite the hesitancy from the frontlines, the National Quality Forum voted overwhelmingly (21 to 2) in January 2023 to include the Severe Sepsis and Septic Shock measure in the FY 2026 HVBP Program. So, what’s their rationale? Let’s take a look.
The Severe Sepsis and Septic Shock measure has been part of the IQR program for some time, and, according to CMS, data has shown that “compliance with the measure was associated with a reduction in 30-day mortality.”
So, the measure works. But it’s not working fast enough. CMS also cites a 2021 report by the Healthcare Cost and Utilization Project, which found that septicemia is still the most frequent principal diagnosis for all non-maternal, non-neonatal inpatient stays. By adopting SEP-1 in the HVBP Program, CMS is showing that it’s now prepared to financially reward hospitals who are making serious strides in the fight against sepsis. With this move CMS has made it clear that SEP-1 is not being removed as an abstracted measure for quite some time – if ever.
CMS also states that it believes that adding the Severe Sepsis and Septic Shock measure to the HVBP Program “will contribute toward CMS’ goal of advancing health equity, as outlined in the CMS National Quality Strategy.” Again, there’s data behind their rationale. The Sepsis Alliance points to multiple studies that show that non-white patients face a higher incidence of sepsis, severe sepsis, and sepsis deaths as compared to white patients.
How the HVBP Sepsis Requirements Will Work
The HVBP Program’s new sepsis requirement is one of 6 measures you’ll have to submit under the program’s Safety Domain:
|
HBVP Program: Safety Domain Measures for FY 2026 |
Current Status |
|
|
CAUTI |
Catheter-Associated Urinary Tract Infection |
Required |
|
CLABSI |
Central Line-Associated Blood Stream Infection |
Required |
|
CDI |
Clostridium difficile Infection |
Required |
|
MRSA |
Methicillin-Resistant Staphylococcus aureus |
Required |
|
SEP-1 |
Severe Sepsis and Septic Shock: Management Bundle |
Required |
|
SSI |
SSI - Colon Surgery |
Required |
The day-to-day implementation of the Severe Sepsis and Septic Shock: Management Bundle measure will work much like it does now under the IQR. But there are four important distinctions to note:
- Baseline period: January 1, 2022, to December 31, 2022
- Performance period: January 1, 2024, to December 31, 2024
- Incentive: Again, this is your opportunity, for the first time ever, to earn a financial reward (not just take a financial penalty) for how well you perform on SEP-1.
- Measurement: Your financial penalty or reward depends entirely on where your hospital falls on the performance bell curve of all hospitals nationwide
Let’s review how each of these could impact you now.
Tip #1: Prepare for The Timelines
Start reviewing your processes, workflows, and data to make sure you’re primed to deliver a successful performance year. Educate your infection prevention and control teams on what this change could mean and why it’s so important to get on the same page.
Tip #2: Refresh Your Memory on HVBP’s Evaluation Method
Up until now, you’ve probably thought “as long as I’m performing at or better than the national average for SEP-1, I’m doing OK.” But the HVBP Program takes the performance of all hospitals nationwide, and then determines your financial gains or penalties based on a which national percentile you fall into.
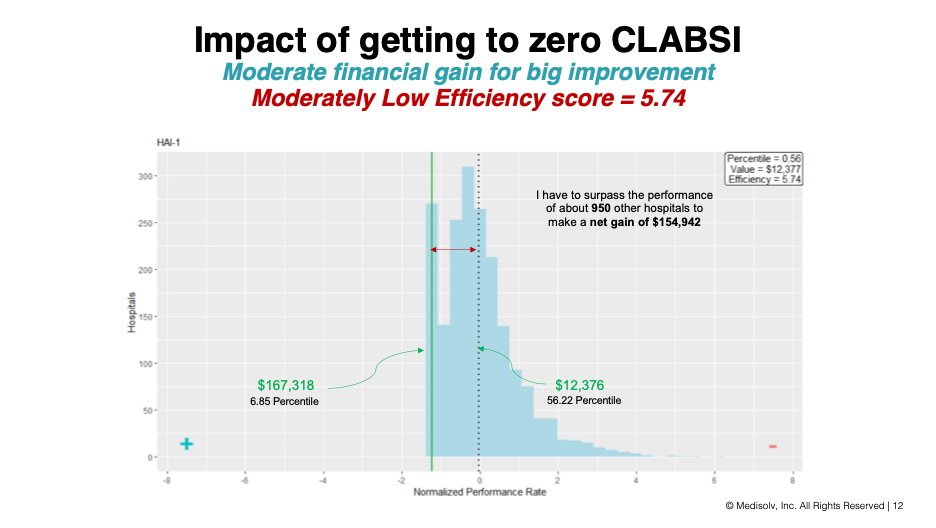
To get a better understanding, let’s use a well-known Safety Domain measure, CLABSI, as an example. Using Medisolv’s Value Maximizer tool, which evaluates the distribution on both the known and forecasted results for all US hospitals to help quality leaders find their most lucrative performance opportunities, we can see that a hospital that currently sits in the 56th percentile for CLABSI can increase its financial gains by nearly $155,000 by getting down to the 6th percentile nationwide...a task that would require outperforming about 950 more hospitals that it currently ranks beneath. This same percentile-based methodology will be used for SEP-1’s payment distributions.
Tip #3: Start Monitoring Your Performance...and Everyone Else’s
Obviously now is the time to reacquaint yourself with your SEP-1 numbers, but you’ll also want to use this time to review your peers’ performance metrics so you can get a sense of where you fall on the national percentile curve. To do this, download the latest SEP-1 data from CMS’s CareCompare. You can also let Medisolv’s Value Maximizer tool do the heavy lifting for you. We’re currently updating it to prepare for the HVBP Program’s adoption of Severe Sepsis and Septic Shock: Management Bundle. Once in place, you’ll be able to forecast your SEP-1 financial performance for up to 3 years out. Contact us if you’re interested in learning more or walking through a free demo.
Best News of All: You Totally Know This Measure Already!
You’ve been doing this measure a long time. You’ve totally got this! With a little reframing of how you evaluate your performance, you’ll be ready to roll. And, as always, Medisolv’s Clinical Quality Advisors are here to guide you through the new requirements if you ever need a pep talk. In the meantime, be sure to check out these additional resources.
- Article: Top Tips: Succeeding with Sepsis (SEP-1)
- Article: What Can Your ED Teach You About Sepsis Care
- Solutions: Value-Based Performance Forecasting
|
Medisolv Can Help This is a big year for Quality. Medisolv can help you along the way. Along with award-winning software you receive a Clinical Quality Advisor that helps you with all of your technical and clinical needs. We consistently hear from our clients that the biggest differentiator between Medisolv and other vendors is the level of one-of-one support. Especially if you use an EHR vendor right now, you’ll notice a huge difference.
|

.png?width=352&name=2026%20Quality%20Reporting%20Deadlines%20Guide%20(1).png)



Comments