What Can Your ED Teach You About Sepsis Care?
Sepsis is the most common cause of death in hospitals in the United States. It also happens to be the costliest condition to treat. Most of the sepsis patients at your hospital are diagnosed with sepsis on arrival, but for your patient population getting sepsis after admission, you will see an increase in mortality rates and costs.
In a study published last year by the Society of Hospital Medicine, researchers concluded that ED sepsis populations fare better in outcomes and timeliness of interventions as compared to hospital sepsis populations.
Here is a quick review of the study’s findings.
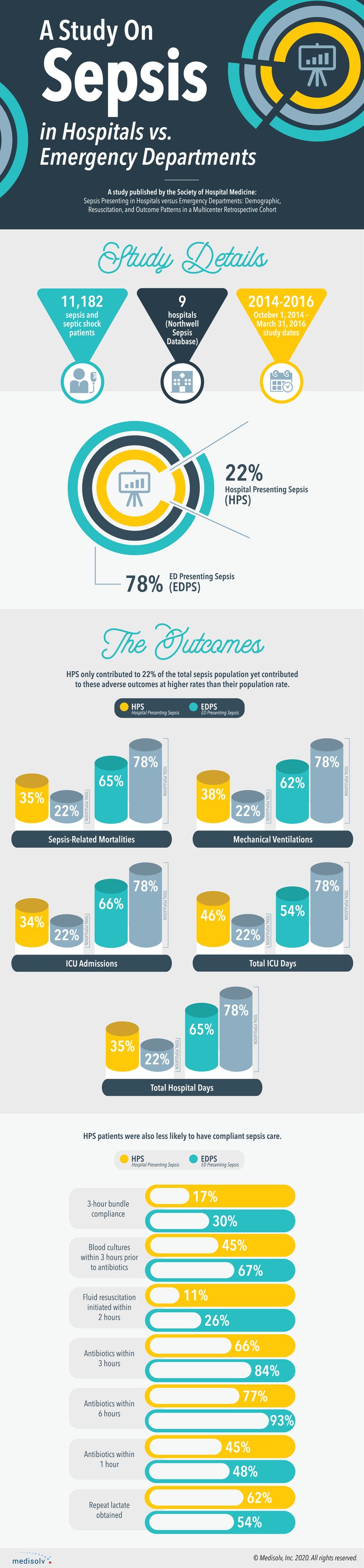
This study concludes that patients presenting sepsis in the hospital have a higher mortality (31.2% vs 19.3%), mechanical ventilation (51.5% vs 27.4%) and ICU admission rate (60.6% vs 46.5%).
HPS patients are connected with longer ICU (five vs nine days) and hospital stays (eight vs 17 days).
They also received sepsis-compliant care less often than their ED equivalents.
So, what can your ED teach your hospital about caring for sepsis patients?
The study attempts to tease out some of these differences by further separating the inpatients into ICU and non-ICU patients. When segmented this way, they observed ICU-inpatients fared better than the non-ICU patients. Focus your quality improvement initiatives around your non-ICU inpatient population.
Conduct a study of your own sepsis patients. Compare your ED sepsis patients to your inpatient sepsis patients. What differences in care do you see? Compare your ICU inpatients to your non-ICU inpatients. Again, note the differences in care. Also analyze the difference in outcomes. Do you see the same adverse outcomes as they found in the study? If so, go back to your differences in care document and observe where the care differed.
In this study, resuscitation disparities account for roughly 25% of the difference in care between the ED and inpatient populations.
There seems to be an additional difficulty in both the recognition and resuscitation of inpatient sepsis patients. Perhaps your inpatients with infections may need closer monitoring as they do in the ED.
Timely resuscitation is strongly associated with better outcomes, which is probably why your ED and ICU patients are faring better. Is there a way to flag at-risk, pre-sepsis patients and put them on a separate care plan?
At the time of this posting the CMS national percentage of patients who received appropriate care for sepsis is at 59%. We are all working to improve sepsis care together, but we know it’s a complicated issue. One technique that works for some may not work for your hospital. By observing what’s actually happening to your specific population you may find some interesting insights that will help you improve your own sepsis care.
If your team could use some help abstracting the sepsis measure, talk to us today about how Medisolv’s abstraction software can simplify this process for you and our experts can guide you through everything you need to know to succeed with this measure.
Sources:
1. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6625440/
2. https://pubmed.ncbi.nlm.nih.gov/28817480/
3. https://www.clinicalmicrobiologyandinfection.com/article/S1198-743X(20)30105-1/pdf
4. https://www.beckershospitalreview.com/quality/10-facts-for-world-sepsis-day.html
5. https://www.sepsis.org/about/its-about-time/
REDUCE THE BURDEN OF ABSTRACTINGMedisolv can help your hospital abstract core measures more timely and accurately. Learn more about ENCOR, our hospital abstracted measure software
|

.png?width=352&name=2026%20Quality%20Reporting%20Deadlines%20Guide%20(1).png)



Comments