Common Pitfalls of PC eCQMs
Maternal health is a top priority for CMS. So much so, that they are requiring the submission of both abstracted and now electronic Perinatal Care (PC) measures for all hospitals eligible to report under the IQR program.
The electronic measures PC-02 (Cesarean Birth) and PC-07 (Severe Obstetric Complications) are relatively new measures which hospitals are required to report starting January 1, 2024. Furthermore, your performance on these measures will be publicly reported for everyone to see on Care Compare.
CMS doesn’t give you a benchmark to shoot for necessarily, but the US Department of Health and Human Services did provide some target goals for these measures in their Healthy People 2030 campaign.
For Cesarean Birth the campaign set a rate goal of 23.6% by 2030.
For Maternal Deaths, the campaign set a goal of 15.7 deaths per 100,000.
The electronic PC measures are complicated. We’ve compiled a list of the common challenges you may face as you implement and improve these measures.
Different EHRs across the delivery lifecycle
Many hospitals have a separate EHR in place for their perinatal care patients and are faced with the challenge of extracting and evaluating data from multiple EHR instances. In this scenario, you’ll need to understand how the data is captured for every data element, understand where that data is stored, if it can be mapped, and how it can be considered for inclusion in the measures.
Consider how to account for this situation. Can you get that data to flow back and forth with an interface or another means to combine the data. You might have to create duplicate documentation fields.
Accurate date and time stamps
The biggest challenge in our opinion, is understanding how reliant these measures are upon precise date and time stamps. As you implement these measures, be sure to consider how date/time stamps are captured (time of documentation vs time of procedure), as well as date/time stamp accuracy.
For instance, the date and time stamp associated with documentation for many of the data elements must be before the delivery date and time. Gestational age, if documented after delivery, will not be considered in the measure evaluation and the patient won’t qualify for the measure denominator. Not capturing this documentation within the date/time requirements could significantly impact your results.
Another common scenario is if clinicians are documenting procedures, such as “cesarean section” in a problem list. The problem list date/times are not always in alignment with the actual procedure date/time. If the date/time entered in the problem list is inaccurate, your results will be too.
The date and time requirements impact many data elements in both measures including due date, gravida, parity, history of birth, and other known conditions like placenta previa.
Determining a source of truth
Just because you have cesarean section documented in the problem list with an inaccurate date and time stamp, doesn’t necessarily mean you’re stuck with bad results. The data elements for these measures are most likely documented in several places in your EHR.
For instance, your hospital probably documents cesarean section in at least one or more of the following: clinical documentation, surgical documentation, and coding. You need to determine where the most accurate date and time of cesarean section is documented, and then put processes in place to use that “source of truth” for your eCQM reports. The source of truth plays a crucial role in the accuracy of your eCQM results.
Take a look at the workflows for each measure below:
PC-02: Cesarean Birth
|
IPP |
Data Element |
Data Capture |
Code Type |
|
Delivery Procedures |
Coding |
ICD |
|
Denominator |
Data Element |
Data Capture |
Code Type |
|
Single Live Birth |
Coding |
ICD |
|
|
Estimated Gestational Age |
Clinical Documentation |
LOINC |
|
|
Delivery Date/Time |
|||
|
Estimated Delivery Date |
|||
|
Gravida = 1 |
|||
|
Parity = 0 |
|||
|
History of Preterm Birth = 0 |
|||
|
History of Term Birth = 0 |
|
Exclusions |
Data Elements |
Data Capture |
Code Type |
|
Placenta Previa |
Coding |
ICD |
|
|
Abnormal Presentation |
|
Numerator |
Data Elements |
Data Capture |
Code Type |
|
Cesarean Section |
Coding |
ICD |
PC-07: Severe Obstetric Complications
|
IPP |
Data Element |
Data Capture |
Code Type |
|
Delivery Procedures |
Coding |
ICD |
|
Denominator |
Data Element |
Data Capture |
Code Type |
|
Estimated Gestational Age |
Clinical Documentation |
LOINC |
|
|
Delivery Date/Time |
|||
|
Estimated Delivery Date |
|
Exclusions |
Data Elements |
Data Capture Workflow |
Code Type |
|
Covid Diagnosis |
Coding |
ICD |
|
|
Covid Related Respiratory Diagnosis |
|||
|
Covid Related Respiratory Procedure |
Coding |
ICD |
|
Numerator |
Data Elements |
Data Capture Workflow |
Code Type |
|
Severe Maternal Morbidity Diagnosis |
Coding |
ICD |
|
|
Severe Maternal Morbidity Procedures |
Coding |
ICD |
|
|
Blood Transfusion |
|||
|
Expired |
Discharge Disposition |
SNOMED |
|
|
Present on Admission |
Coding |
Present On Admission |
Also note the places where you can choose from multiple EHR sources to capture the data element listed. Determine which is the source of truth and implement your reports in a way that captures that data and ignores the rest.
We have found that capturing the data in clinical documentation is the most accurate way to get the data element as well as the true date and time needed.
Risk-adjusted variables
PC-07 has even more to consider than what you see listed above because this measure is risk-stratified. CMS wants to consider how sick your patients were before delivery by evaluating the presence of certain conditions and whether or not they were present on admission. You need to be prepared to include up to 29 (!) separate variables with your PC-07 QRDA I files for submission.
Here’s a list of those variables.
- Anemia
- Asthma
- Autoimmune Disease
- Bariatric Surgery
- BMI >=40
- Cardiac Disease
- Economic Housing Instability
- Gastrointestinal Disease
- Gestational Diabetes
- HIV
- Hypertension
- Maternal Age (derived from birthdate)
- Mental Health Disorder
- Multiple Pregnancy
- Neuromuscular Disease
- Other Pre-eclampsia
- Placenta Previa
- Placental Abruption
- Placental Accreta Spectrum
- Pre-existing Diabetes
- Preterm Birth
- Previous Cesarean
- Pulmonary Hypertension
- Renal Disease
- Severe Pre-eclampsia
- Substance Abuse
- Thyrotoxicosis
- Long-term Anticoagulant Use
- Obstetric VTE
You must ensure these conditions are captured in your EHR, or both EHRs (see first challenge above) and that they are documented as present on admission (if applicable). You will need to have a way to validate, review, and track a patient’s risk variables throughout the reporting year and definitely in advance of submission. Not capturing and/or submitting these variables in association with patients who qualify for this measure will impact your risk adjusted score and not necessarily reflect the severity of illness of your maternal patient population.
Shared value set codes
One final challenge to consider is that within these measures there are data element value sets that contain the same codes. For instance, the value set for Cesarean Birth and the value set for Delivery Procedures share the code for Cesarean section (procedure):
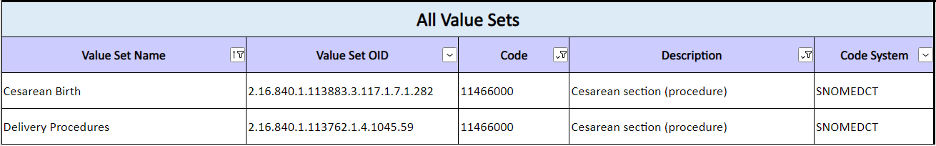
When a code is shared liked this, implementing the eCQM logic correctly is difficult. The logic gets confused because it doesn’t understand which data element the code goes with. Go through your mapping, review your codes, and make sure you are using different codes for each required data element. Each value set has other codes that aren’t shared, use those to capture this information.
How to be successful with your PC measures
Reviewing the challenges above is a good start if you want to be successful with these measures. Consistent troubleshooting of measure performance overtime will bear fruit. You’ll start feeling confident in the accuracy of your results and then can begin the real work of quality improvement to ensure you are taking good care of your patients.
In addition to consistent troubleshooting, here are some suggestions from our clients with the best PC measure results:
- Our most successful clients have been working on these measures for years. Start early and work on them often.
- Compare your electronic PC measure results to your abstracted PC measure results. Understand where you have different patient populations and results, use that information to guide your troubleshooting.
- Stay on top of changes to the measures. Meet on a regular cadence with your Medisolv advisor, stakeholders, and resources. Your Medisolv advisor will give you the information you need to know about measure changes.
- If you aren’t a client, you’ll need to make sure you are reading every proposed and final rule from CMS. In May, CMS releases new specifications and value sets for these measures for the next year. You’ll need to review these for changes to logic and value sets and adjust your workflow and mapping as needed.
- Provide feedback to clinicians if they aren’t documenting in accordance with the workflow and/or protocols. Plan for re-education. Implement a peer review process. The more you share results the more they will understand where they can improve.
- Request feedback from clinicians, test something new and go back and adjust again. These are relatively new measures so you can assume you’ll need to make adjustments. Give yourself enough time to adjust, test, get clinician feedback, readjust, and monitor for improvement.
- Work with your vendors and resources. Submit concerns, ask questions, open JIRA tickets. CMS is listening and does incorporate changes based on feedback.
- Educate and communicate the “why” up and down your organizational structure.
This last point above is the most important when it comes to actually making progress with these measures and decreasing rates. It’s a mindset shift for you as a quality leader. CMS wants you to use your eCQMs to change your results and improve your rate even if there isn’t a specific threshold you’re aiming for.
A reduction in Cesarean-Sections means an increase in patient safety, a decrease in maternal and neonatal morbidity, cost savings, a decrease in repeat c-sections, a decrease in morbidity in future births. The same can be said for the severe obstetric complications measure and shockingly CMS explains that a considerable amount of maternal morbidity and mortality events could be prevented.
It's up to you as a quality leader to lead the charge in changing the outcomes for our country’s moms and babies. And we are here to assist you in this mission.
Medisolv Can HelpThis is a big year for Quality. Medisolv can help you along the way. Along with award-winning software you receive a Clinical Quality Advisor that helps you with all of your technical and clinical needs. We consistently hear from our clients that the biggest differentiator between Medisolv and other vendors is the level of one-of-one support. Especially if you use an EHR vendor right now, you’ll notice a huge difference.
|

.png?width=352&name=2026%20Quality%20Reporting%20Deadlines%20Guide%20(1).png)



Comments