dQMs: Preparing for the Unknown
The acronym dQM has been floating around the healthcare sphere more regularly since CMS put their intention to go completely digital by 2025 in the last IPPS final rule. I’ve found that these measures generally evoke two reactions: either someone is frightened by the implications of this transformation, or they scoff at what seems to be an unrealistic timeline.
Let’s review what dQMs are and provide you some details into the work you’ve already done in this area to make this goal more realistic for both parties.
What is a Digital Quality Measure (dQM)?
You have to do a bit of searching out there to find an official definition, so I’ll provide a link to the CMS definition as provided on a recent webinar.
Essentially, dQMs must originate from sources of health information that are captured electronically and can be transmitted electronically via interoperable systems. It’s an all-encompassing definition. dQMs must automatically pull data generated during the normal course of care and provide the ability to measure and aggregate quality data across all levels of the delivery systems.
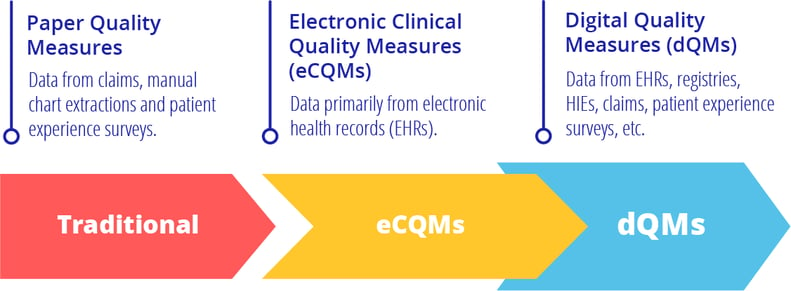
This sounds a lot like something you do already. eCQMs (Electronic Clinical Quality Measures) are a form of dQMs. (So that’s good news). CMS distinguishes eCQMs as a subset of dQMs. eCQMs are calculated using data pulled automatically from the EHR. That’s the difference. eCQMs are sourced from the EHR. dQMs are sourced using any health information such as an EHR, claims, registry or similar.
CMS’ Plan to Transform to Digital Quality Measurement
CMS intends to transform the way the industry measures the quality of patient care by 2025 as outlined in the CMS Quality Measurement Action Plan. They want to use data and information as essential aspects of a healthy, robust healthcare infrastructure to allow for payment and management of accountable, value-based care and development of learning health organizations.
They’ve outlined 5 goals of this plan.
- Use Meaningful Measures to streamline and align quality measurement
- Leverage measures to drive improvement through public reporting and payment programs
- Improve quality measure's efficiency by a transition to digital measures and use of advanced data analytics
- Empower consumers to make the best healthcare choices through patient-directed quality measures and public transparency
- Leverage quality measures to promote equity and close gaps in care
To achieve those lofty goals there are some specific tasks that must be executed.
- Accelerate development and testing of eCQMs using FHIR API technology for transmitting and receiving quality measurement
- Transform data collection to use FHIR API technology and all CMS data (all-payer data)
- Utilize a data-driven framework to assess measure priorities and performance
- Leverage centralized data analytic tools to examine programs and measures
- Evaluate new technologies for advanced machine learning and neural networks
- Expand the availability of public use files for CMS data by 2021
The FHIR technology seems to be the crucial factor determining whether we will get there by 2025. FHIR API would allow data to flow in and out of systems more seamlessly than the various, clunky ways that it happens now. FHIR would take a lot of the customization out of this process and standardize it. Think about how everyone can open a PDF file on their computer. The point of a PDF file is to allow universal access to a document. The point of a FHIR API is to allow universal access to health information.
Also see: FHIR for the Busy Quality Director
Most of the experts I’ve talked to on this subject agree that FHIR isn’t quite there yet. It would be a stretch to believe we can make such extraordinary progress on this in three years that would allow EVERYONE to use FHIR API for connection.
Take a look at this graphic below. It summarizes visually what CMS is trying to do. They want to simultaneously advance technology (FHIR), align measures (Meaningful Measures campaign), improve data quality (get data from all electronic sources) and optimize data aggregation (publicly report it on Care Compare).
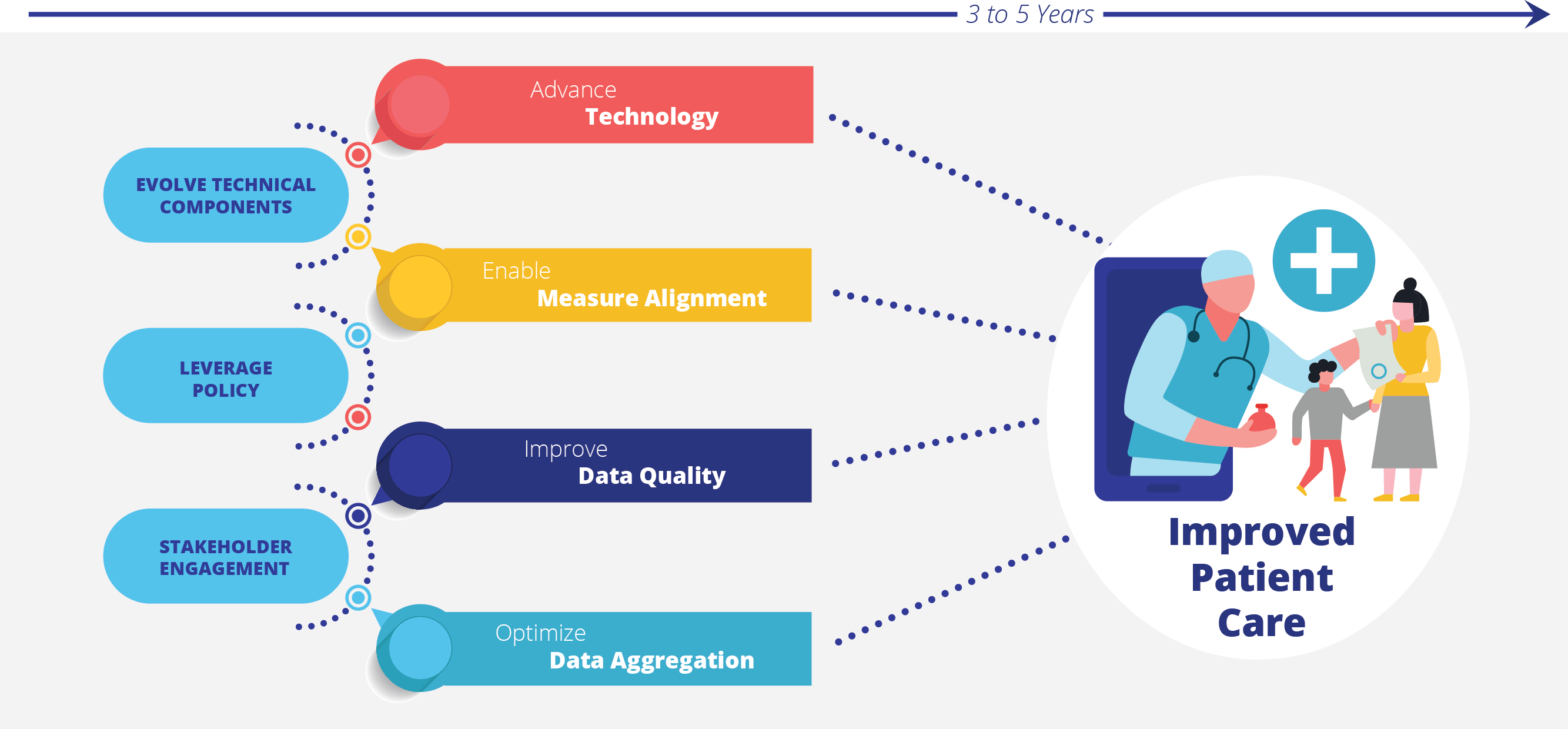
It’s easy to see why CMS is pushing for this. Digital measurement is truly the future of healthcare. They want to enable a future that is completely electronic using standardized interoperable data. This will (eventually) reduce the burden on healthcare systems both from a technical and resource standpoint. They want this data to be quickly available so healthcare leaders can use it to improve care and consumers can understand the choices they have.
Challenges of dQMs
I’ve probably painted a rosy picture of what the future of quality measurement could look like. Here’s the reality of what we must overcome to meet that 2025 goal.
The biggest challenge I foresee is getting access to everyone’s data in that timeframe. If you just had to connect the big health systems and practice networks there might be a chance. They generally have a more interconnected system. But what about the standalone practices with homegrown EHR technology? Or a critical access hospital whose patient population doesn’t have reliable access to internet. How are we going to ensure these population types are counted in this initiative?
It brings us back to the health equity measurement problem. Are we only evaluating patients in either rich or urban populations and how does that skew the data of what quality of care we provide the American population?
How can we get data from all sources to provide a holistic view of care?
Beyond technological inequities, there is a component of resource scarcity as well. If you are part of a big health system or a large ACO network, the prospect of getting all healthcare sources of data online across all your patients may seem daunting, but you probably have more manpower to handle this type of initiative. A small hospital or practice may be struggling already with an overstretched IT team (or person!) that is responsible for every aspect of their connectivity (including a broken-down printer). There might be one quality leader dedicated to overseeing patient care. Asking them to engage in advanced analytics sounds pretty stupid.
The Progress We’ve Already Made
Now have I crushed your aspirational goals? Ok, let’s start again. Think back to 2008. This journey toward electronic measurement started nearly 15 years ago. Remember in 2008 how most of the country still used paper charts and there were virtually no EHRs that talked to each other? We thought getting small and underserved health care systems online seemed like an impossibility in 2008.
Now look at the progress we’ve made in that time. eCQMs weren’t even invented and over the course of 15 years, they were initiated with the Meaningful Use program, flourished in many of the regulatory programs (IQR, OQR, QPP) and have further expanded into the new hybrid measures (which combine claims and EHR data to calculate measure performance).
The good news is that we’ve been on this journey together for a while and you’ve done a lot of work along the way.
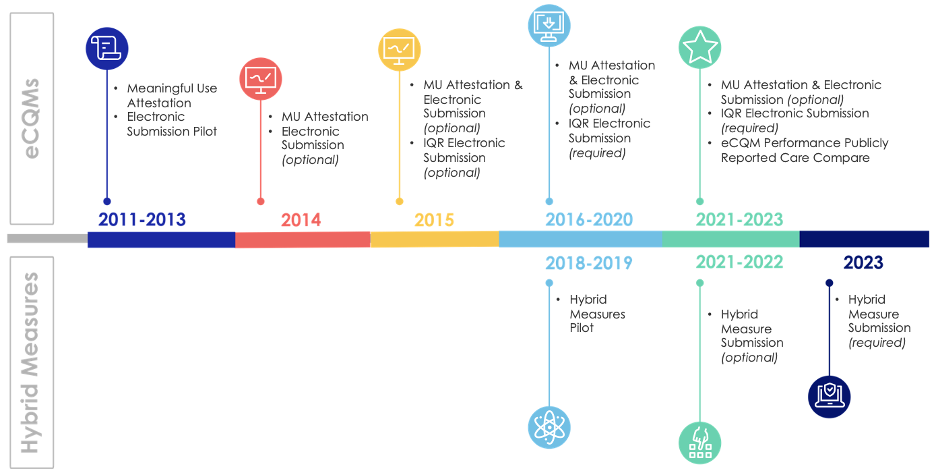
You can think about moving to dQMs as just another step in the journey.
dQM Readiness
The time is now for you to begin thinking in earnest about how your organization can move to dQMs by 2025.
- Engage and participate: Don’t be the straggler. Start evaluating your data sources and identifying where you have digital data gaps now.
- Develop an effective team structure: If you don’t have it already, ensure you have a multi-disciplinary team set up for this type of work. The team should involve Quality leadership, IT leadership, clinician and executive stakeholders.
- Partner with the right third-party vendors: This includes making sure you have the right EHR in place and yes, in our opinion, working with a company like Medisolv whose entire company is built on digital measurement is a good way to ensure you have a team of people who can get you there by 2025.
- Start now to be ready in the 2023 reporting cycle. It sounds early but it will take at least two years to identify your gaps and work to overcome the challenges we talk about above.
There are a couple of lessons learned I’d like to point out. Keep these in mind as you plan for the future.
Implement a comprehensive data management system that allows you to seamlessly acquire and aggregate data sources. You may need to work with a vendor who can identify sources and help you understand where you need to map in your EHR in order to get the quality measures you need.
Plan for ongoing data management. This is not a one-time effort. Nor is this a once-a-year project. You’ll need to plan for regular incremental data updates. Create a process to update source data changes without interruption.
Optional participation is key. For instance, the hybrid measures (readmission and mortality) are both optional to submit this year but required next year. We strongly suggest you participate in these optional measures when CMS puts them out there. They will provide you a lot of information about your performance that you can use to improve before they are required and publicly reported.
New and updated measure specifications should be in place at the beginning of a performance period so you can start measuring quality on January 1. We often hear clients frustrated over this one. Many EHRs aren’t ready until much later in the year which puts you at a disadvantage. Don’t sit patiently by. Reach out to your EHR and express your need for timely updates. If enough of their clients complain they will be forced to do something about it.
Build time buffers in your plan. It always takes longer than you initially estimated. That’s why we encourage you to begin by 2023.
Digital Quality measurement is a journey we all started nearly 15 years ago. Your upfront investment in this transformation will yield benefits down the road. There will be better care coordination for our patients. Eventually the costs will be lower. Patients, healthcare organizations and CMS will benefit from a greater level of transparency. You’ll be empowered to make better decisions with actionable real-time data. Hopefully we will see better patient outcomes and importantly we can allow our healthcare consumers to make informed decisions about their care, which provides a greater level of accountability to our healthcare system.
Medisolv Can HelpAlong with award-winning software, each client receives a dedicated Clinical Quality Advisor that helps you with your technical and clinical needs. We consistently hear from our clients that the biggest differentiator between Medisolv and other vendors is the level of one-of-one support. Especially if you use an EHR vendor right now, you’ll notice a huge difference.
|

.png?width=352&name=2026%20Quality%20Reporting%20Deadlines%20Guide%20(1).png)



Comments