How does the IQR Penalty Work?
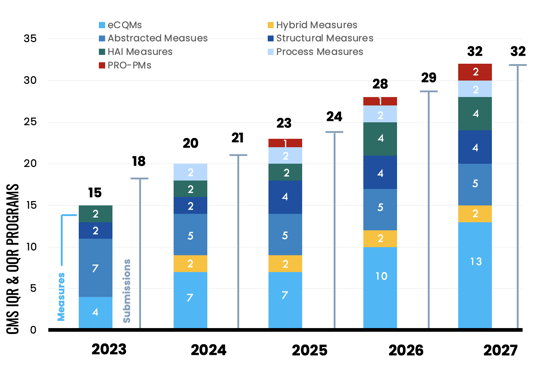
In the next few years, Quality leaders must report a slew of new required measures to the CMS Inpatient Quality Reporting (IQR) program.
All of these measures are publicly reported and missing even one measure, one submission, one time will result in a failure to successfully meet your reporting requirements, which has financial consequences. CMS penalizes hospitals that fail to meet their IQR requirements, resulting in an Annual Payment Update (APU) reduction to their Market Basket Update (MBU).
Phew! That’s a lot of pressure on a quality leader.
In this article, we focus on the Inpatient penalty only and explain the financial implications of not successfully meeting IQR program requirements.
The Penalties
Under the IQR program, hospitals that do not meet the requirements face a penalty of a 25% reduction to their Market Basket Update. This reduction is applied to the annual reimbursement amount that hospitals receive for claims billed to Medicare.
The Math
To illustrate the financial impact, let's consider a hypothetical scenario:
- Your hospital bills Medicare $100,000,000 annually.
- You do not successfully meet your IQR requirements.
- In 2026, CMS provided a Market Basket Update of 2.6%.
- Assuming you bill Medicare a similar amount, you would have received Medicare claims reimbursements of $102,600,000.
- ((100,000,000 x .026) + 100,000,000) = $102,600,000
- However, due to the penalty, you only receive a 1.775% increase (a 25% reduction to the Market Basket Update), resulting in $20,834,739.
- ((100,000,000 x .01775) + 100,000,000) = $101,775,000
|
Base Revenue |
$100,000,000 |
||||
|
Passed APU |
MBU |
Year |
Would have Received |
Received |
Lost Revenue |
|
N |
2.6 |
2026 |
$102,600,000 |
$101,775,000 |
$825,000 |
How the Penalty is Calculated
Hang on. If I reduce 2.6% by 25%, I come up with 1.924%. You applied 1.775%. That’s because there are a couple of steps CMS takes to assess the penalty.
Every year, CMS gives hospitals under the Inpatient Prospective Payment System (IPPS) a Market Basket Rate-of-Increase. You can think of it like a cost-of-living increase. It's the new payment rate CMS will pay your hospital for the costs you incur servicing their beneficiaries. They then assign a productivity adjustment, which gives you the final rate of increase you receive if you meet all your IQR and Promoting Interoperability (PI) requirements (see "Submits Quality Data and is a Meaningful EHR User" column in chart below).
"Hospital Submitted Quality Data" = successfully completed the IQR Program Requirements.
"and is a Meaningful EHR User" = successfully completed the PI program requirements.
If you don’t meet your IQR requirements (i.e., “Did NOT Submit Quality Data and is a Meaningful EHR User”), your 25% reduction comes off the 3.3% first, then they apply the productivity adjustment decrease (column four below).
| FY 2026 Applicable Percentage Increases for the IPPS | ||||
| FY 2024 | Hospital Submitted Quality Data and is a Meaningful EHR User | Hospital Submitted Quality Data and is NOT a Meaningful EHR User | Hospital Did NOT Submit Quality Data and is a Meaningful EHR User | Hospital Did NOT Submit Quality Data and is NOT a Meaningful EHR User |
| Market Basket Rate-of-Increase | 3.3 | 3.3 | 3.3 | 3.3 |
| Adjustment for Failure to Submit Quality Data under Section 1886 (b)(3)(B)(viii) of the Act | 0.0 | 0.0 | -0.825 | -0.825 |
| Adjustment for Failure to be a Meaningful EHR User under Section under Section 1886 (b)(3)(B)(xi) of the Act | 0.0 | -2.475 | 0.0 | -2.475 |
| Productivity Adjustment under Section 1886 (b)(3)(B)(xi) of the Act | -0.7 | -0.7 | -0.7 | -0.7 |
| Applicable Percentage Increase Applied to Standardized Amount | 2.6 | 0.7 | 1.775 | -0.7 |
IQR Penalties in 2026
In 2026, CMS provided an MBU update of 3.3%. If you fail to meet your IQR requirements in 2026, you will only receive a 1.775% increase instead of the full 2.6% (the increase minus the productivity adjustment). And remember, this is just your IQR requirements. There are other CMS programs that you could potentially be reporting to and that CMS could further penalize your hospital.
CMS provides the yearly Market Basket Update in the IPPS Proposed Rule (around April) and finalizes it in the IPPS Final Rule, which comes out around August each year. I’ve pulled out the specific pages that address the Market Basket Update for 2026 in a PDF link below. Additionally, I’ve pulled the historical MBU for the IPPS (IQR) and other CMS programs.
- Market Basket Update Historical Review
- 2026 IPPS Final Rule MBU Section
- FAQs: Market Basket Definitions
The financial impact of not meeting IQR program requirements can be significant for hospitals. The penalties imposed by CMS make it crucial for quality leaders to get the support they need to successfully meet their reporting requirements.
If you’re concerned about keeping on top of everything this year, consider reaching out to us. We complete your hospital’s submission to the IQR, OQR, IPFQR, and TJC ORYX® programs. You'll never miss a submission deadline.
We also provide ongoing education to help you understand the final rules and explain exactly what you need to do to be ready for the applicable reporting year.
Medisolv Can HelpAlong with award-winning software, each client receives a dedicated Clinical Quality Advisor that helps you with your technical and clinical needs. We consistently hear from our clients that the biggest differentiator between Medisolv and other vendors is the level of one-on-one support. Especially if you use an EHR vendor right now, you’ll notice a huge difference.
|

.png?width=352&name=2026%20Quality%20Reporting%20Deadlines%20Guide%20(1).png)



Comments