The Hybrid Readmission Measure: Understanding How It Works
Have you heard about the new hybrid measure from CMS? In the 2020 IPPS final rule, the hybrid measure goes from voluntary to mandatory by 2023. And what’s more is that your measure performance will be publicly reported on Hospital Compare shortly thereafter.
If you missed it last year, CMS held a pilot program for the hybrid measure. They received 150 successful submissions to the program. Sixty-nine of the 150 submissions to CMS were completed by us here at Medisolv!
We learned a lot from the files we submitted on our clients’ behalf and now 69 of our hospitals are ready to easily fulfill their hybrid measure requirements when the time comes.
In this blog, I thought I would provide you an overview of the hybrid measure so you can begin thinking about how you can succeed with this new measure type in the future.
Hybrid Measure Timeline
By 2023 the Hybrid Hospital-Wide 30-Day Readmission (HWR) measure will be required as a part of your IQR requirements.
| Voluntary Measurement Period |
| July 1, 2021 – June 30, 2022 |
| July 1, 2022 – June 30, 2023 |
| Mandatory Measurement Period |
| July 1, 2023 – June 30, 2024 |
| Results Posted to Hospital Compare |
| July 2025 |
How to set up a Hybrid measure
The truth is, if you have good mapping in your EHR already, the process shouldn’t be that difficult for you.
This video below gives a good, high-level summary of the hybrid measure. It’s about 10 minutes long, but it will explain the measure in simple terms for you.
If you don’t have time to watch the video, here is a quick written summary.
Also See: What is the Hybrid Readmission Measure?
How the Hybrid Measure is Captured
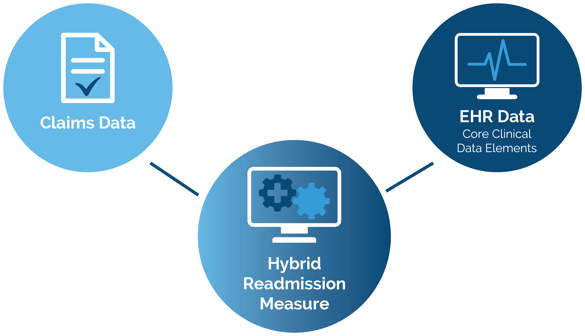
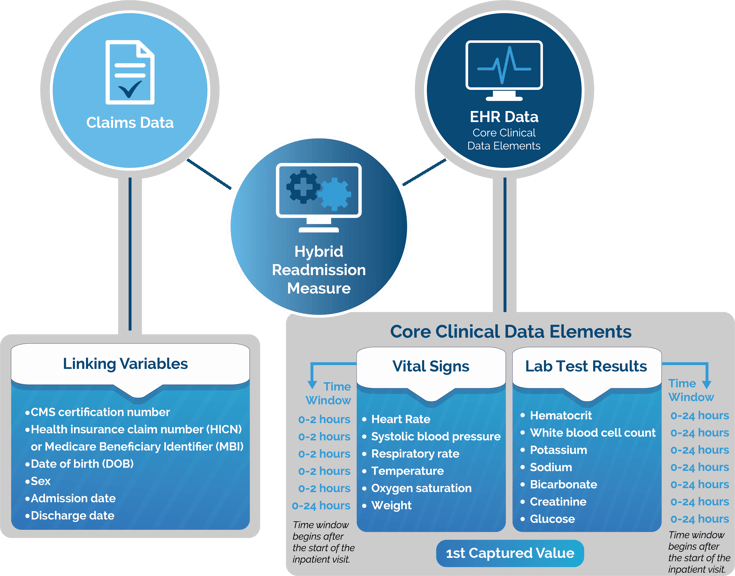
To explain, I’ll use the Hybrid HWR measure as our example. The traditional claims-based Hospital-Wide 30-Day Readmission measure is calculated based on the claims data that you submit to CMS. The new Hybrid HWR measure uses that same claims data but supplements it with an electronic file that contains Core Clinical Data Elements (CCDE) such as patient vital signs and lab results.
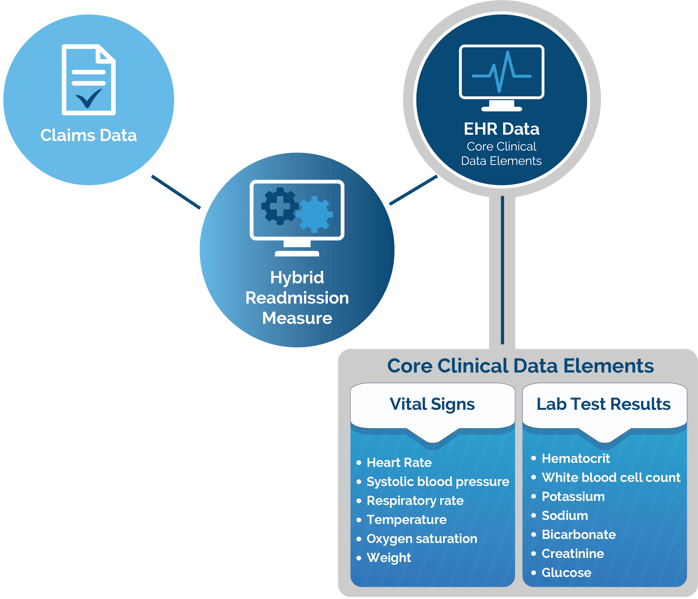
There are 13 CCDE that you need for the HWR measure. They consist of six vital signs and seven laboratory test results. You must map these 13 CCDE to your EHR. See the 13 CCDE in the graphic below.
Once CMS receives your electronic data they will use six linking variables to match the patient EHR data to the claims data.
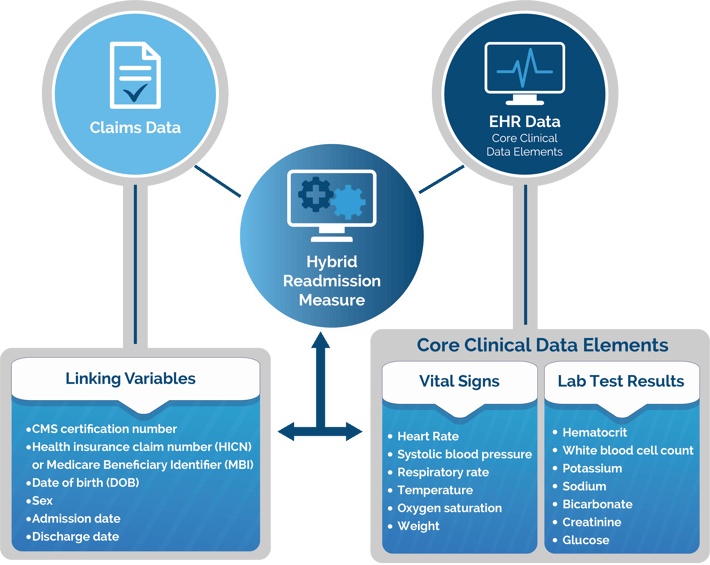
This produces the Hybrid measure.
How the Hybrid Measure is Calculated
CMS will use both sets of data to risk adjust the patient. By risk adjusting, they intend to understand how sick the patient was at the time they were first admitted to your hospital. In order to complete this adjustment, you must submit the electronic data that adheres to the specifications just like your normal eCQMs.
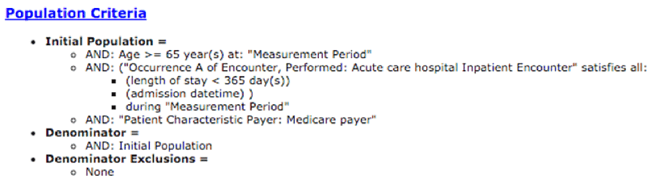
This electronic portion of the hybrid measure is much simpler than your other eCQM specifications. You can check out the logic here. The Initial Patient Population is all inpatients that are 65 or older who have Medicare as their payer. The Denominator is the same and there are no Exclusions.
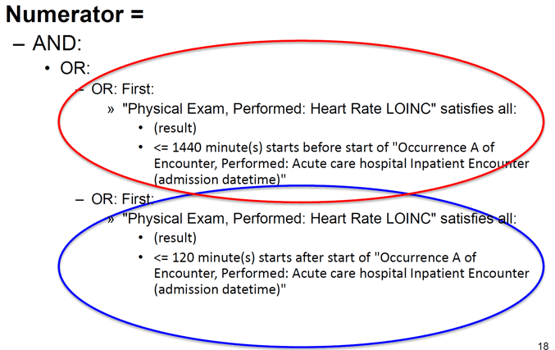
The Numerator can be satisfied by capturing the earliest instance of at least one of the 13 core clinical data elements within these required time frames:
*Additionally, there is look back logic to evaluate the 1st captured value if completed 0-24 hours before the start of the inpatient visit.
The numerator is just a bunch of "OR" statements indicating that any one of the data elements that you map will meet the measure requirements. It's fairly simple to validate. As long as each patient has at least one captured value within the allotted time frame then they make it into the numerator.
Submitting the Hybrid Measure to CMS
You are responsible for submitting the electronic file. There is no additional submission for the claims data. You must submit the electronic portion like you would your normal eCQMs. You must generate and submit the QRDA I file to CMS.
CMS will then risk adjust your patients based on the claims and electronic data using their models.
At Medisolv, we help clients map these data elements to their EHR, produce their QRDA I file, submit the file to CMS and help resolve any rejections. We are pretty proud that we submitted nearly half of the hybrid measures to CMS as a part of the pilot program and our hospitals should be proud as well.
If your organization also wants to be a Quality trailblazer, talk to us today about how we can work with you to create an innovative and comprehensive Quality program at your organization.
Free Download:
The Hybrid Measure Implementation Guide:
How to Implement the Hybrid Readmission Measure
The new hybrid readmission measure is moving from voluntary to mandatory over the next several years. This guide explains all about the hybrid measure – how it is captured and mapped in your EHR and how CMS will calculate your measure performance.
This guide explains:
- What a hybrid measure is
- How hybrid measures are captured and mapped in your EHR
- How CMS calculates your hybrid measure performance
- The timeline for reporting hybrid measures to CMS
|
|


.png?width=352&name=2026%20Quality%20Reporting%20Deadlines%20Guide%20(1).png)



Comments