The Difference Between MIPS 2017 vs MIPS 2018

The beginning of the year can be a tricky period for those responsible for overseeing the smooth execution of their Quality program. At this point in the year you may not yet have submitted your files to successfully meet your 2017 MIPS requirements, but the new year has started, and with it, the need to start monitoring and capturing your results for your 2018 MIPS reporting year.
During this time we thought it would be helpful to clearly lay out the differences in the MIPS program between 2017 and 2018. This way, while you are preparing to submit your required MIPS files (APRIL 2 DEADLINE), you can keep in mind the measures you should be tracking and monitoring in 2018.
Let's review how the MIPS program changes or stays the same in 2018.
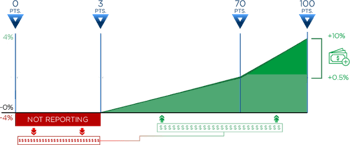
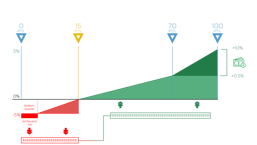
PAYMENTS
|
|
|
|
-4% / +4% Eligible Clinicians can lose -4% if you do not achieve the score threshold of the MIPS program or gain up to 4% for excellent performance. |
-5% / +5% Eligible Clinicians can lose -5% if you do not achieve the score threshold of the MIPS program or gain up to 5% for excellent performance. |
Note: This payment adjustment will be made to your fiscal year 2019 and 2020 Medicare fee schedule respectively.
Score threshold requirements
In 2017, all clinicians really have to do is the bare minimum (submit one measure with information for one day) and they will score three points and avoid a penalty. In 2018, you must actually do a little bit more work to achieve the 15-point threshold.
|
|
|
|
Must achieve a score of
|
Must achieve a score of
|
By scoring at least 70 points in either 2017 or 2018, you’ll be eligible for the Exceptional Performance bonus money. CMS has set aside an additional $500 million to distribute to anyone who scores between 70 – 100 points (see far right). This is on top of whatever portion of money you receive from those who do not meet the threshold (in red).
CATEGORY REQUIREMENTS
There are four categories that make up the MIPS program.
 |
|
|
 |
|
Quality (Formerly the PQRS program) |
Advancing Care Information |
Improvement Activities (New program) |
Cost (Formerly the |
Each of these categories carries a different weight. Your score in each category will be totaled into one composite MIPS score. The weight that each category carries differs between 2017 and 2018.
|
|
|
|
|
|
For the first time in 2018, your Cost performance will factor into your total MIPS score. To balance the total score, they reduced the weight of the Quality category to 50%.
QUALITY CATEGORY
|
|
|
|
Maximum Points: 60 points Requirements
|
Maximum Points: 60 points Requirements
|
Data Completeness
|
|
|
|
50% Submitted Quality measures must contain at least 50% of all Eligible Clinician patients across all payers. |
60% Submitted Quality measures must contain at least 60% of all Eligible Clinician patients across all payers. |
ADVANCING CARE INFORMATION CATEGORY
|
|
|
|
Maximum Points: 155 possible points, but capped at 100 points Requirements
|
NO CHANGE |
Note: If you have achieved Meaningful Use Stage 3 Functionality and have the 2015 EHR Certification you may choose to submit the advanced Base measure set instead.
Improvement Activities CATEGORY
|
|
|
|
Maximum Points: 40 points Requirements
|
NO CHANGE |
Note: If you are Patient-Centered Medical Home and more than 50% of your practices are recognized as a PCMH, you automatically receive full credit for this category.
Cost CATEGORY
|
|
|
|
Maximum Points: 0 points Requirements
|
Maximum Points: Unknown Requirements
|
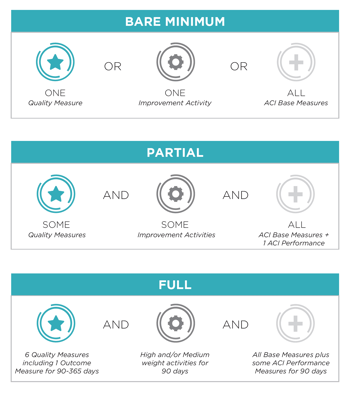
Reporting Options
In 2017, you could "Pick Your Pace" for reporting to CMS. In fact, it takes very little effort to simply avoid the penalty. Alternatively, you could fully participate in 2017 and if you do so, you will be much more prepared to handle the requirements of 2018. In this year, there is no option for going at your own pace. You must attempt to fulfill all of the requirements and based upon your performance, you will receive a total MIPS score that will ultimately give you a pay increase or decrease.
|
|
|
|
Pick Your Pace
|

Quality
Advancing Care Information

Cost
|
Whether you are all wrapped up for your 2017 reporting or are still scrambling to figure out what you need to do, take the time now to ensure your organization has a good plan in place. Identify all of the players and stay in regular communication about goals and timelines. Find your vendor (like Medisolv) who will help you with your performance improvement in addition to submitting your files. The only way to have a comprehensive Quality program in place is to ensure every detail is thought through. The beginning of the year is a good time to clear your head, put new processes in place and start fresh.
DOWNLOADS:
Beginner's Guide to MACRA (2017) |
Beginner's Guide to MIPS Year 2 (2018) |




.png?width=352&name=2026%20Quality%20Reporting%20Deadlines%20Guide%20(1).png)



Comments