It's Coming for Us All: Sepsis
.gif?width=900&height=600&name=Sepsis-Map%20(002).gif)
What is this a picture of?
Is it:
- A map of the New York subway system
- Death Star blueprint plans
- A graphic interpretation of a black widow spider web
- Healthcare's attempt to improve patient care
As you may have guessed from the title of this post, we are talking about sepsis. And if you know anything about sepsis, you may have deduced that this is actually a view of the sepsis algorithm logic that makes up the CMS Core measure, SEP-1 Early Management Bundle, Severe Sepsis/Septic Shock.
Since CMS began requiring that hospitals collect data on this measure in October of 2015, it has been … how do I put this … less than popular.
Why? Well, for starters, it’s complicated!
According to Mayo Clinic, sepsis is on the rise in America. As such, CMS created a measure to help hospitals and providers properly document and treat sepsis. “By providing timely, patient-centered care and making sepsis care more affordable through early intervention, this measure can result in reduced use of resources and lower rates of complications.”1
But sepsis isn’t as straightforward as say the PC-01 Elective Delivery measure. Christopher Seymour, MD, of the University of Pittsburgh School of Medicine, explained the complications with sepsis, “There is no single characteristic that identifies septic patients, and that’s what makes it such a challenge.” However, he added, “Sepsis is under recognized and underdiagnosed, and anything we can do to promote doctors and hospitals to take better care of patients with sepsis is serving the greater good.”2
In addition to this, timing is a critical component of the sepsis measure. Different activities need to be completed within three or six hours of diagnosis. And these activities vary based on whether you are talking about severe sepsis or septic shock. The difficultly of diagnosis, paired with the timing elements, creates a very complicated and lengthy algorithm that an abstractor must follow to assess whether the patient was properly cared for according to the SEP-1 measure.
For comparison’s sake, let’s look at a different Core measure algorithm. This is the algorithm for STK-10 Assessed for Rehabilitation.
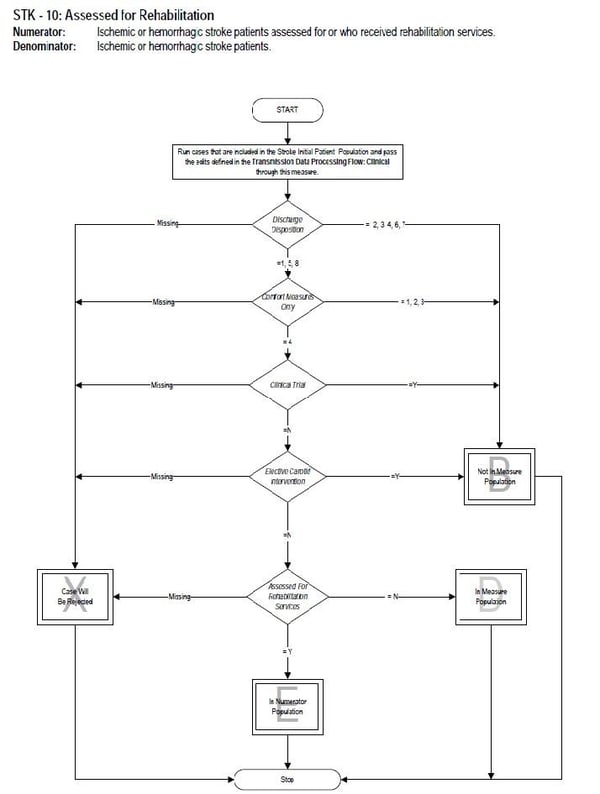
Hmm. I see a few differences between the measure logic algorithms.
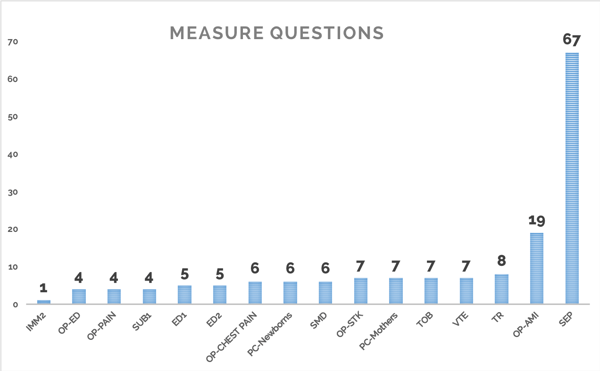
Aren’t convinced? Let’s take a look at the difference in the number of possible questions that an abstractor could have to answer for the sepsis measure as compared to other current Core measures.
Ok, I’m sure that I’m not telling anyone anything they don’t already know. Sepsis has been a pain in the neck for quite some time. So why did I bring up such a painful topic? Because, starting in July of this year, your hospital’s sepsis performance will be publicly reported on Hospital Compare.

That’s right. Starting in July of 2018, Hospital Compare will release your hospital’s 2017 sepsis performance. They will begin with data from Quarter 1 (Q1) through Quarter 3 (Q3) of 2017. There will be a preview period for hospitals that is anticipated to be from May 4 – June 2, 2018. The actual release date is scheduled for July 25, 2018.3
Then, at the start of each new quarter, another quarter’s worth of information will be released, and the oldest quarter will be removed, so a full rolling year’s worth of data is published. That means that in October of this year, CMS will add your 2017 Q4 data to Hospital Compare.
How ready is your hospital for this information to be displayed to the general public? Since it has never been published before, we don’t know how the average hospital is performing. It will be interesting to see what the average sepsis score is nationwide.
It’s essential that hospitals invest time into figuring out how to improve their sepsis results. If you ask the average abstractor what they think about the sepsis measure, they will probably spit out a few choice curse words. Make sure you are providing them with the best tools to efficiently abstract this measure. For example, Medisolv’s ENCOR software makes abstraction simpler with advanced worksheet logic that guides the abstractor through the sepsis measure.
Even if your team has all of the right tools, the sepsis measure can still be challenging. Successfully reporting sepsis doesn’t just require abstracting the measure quickly to get feedback to leadership about daily performance; it also involves improving that performance. Getting physicians and clinicians to properly document sepsis can be a challenge.
So, the best advice we can give you is to make sure someone on your team takes the lead on this initiative. CMS provides webinars on sepsis with frequency. Make sure to attend those webinars. The Quality Reporting Center also has many resources to help hospitals succeed with this measure. And, as painful as this may sound, it will help if you go through the measure logic carefully to make sure you fully understand how this measure is calculated.
By being proactive and making sepsis performance improvement a priority, you are sure to see increased performance results over time.
If your team could use some help abstracting the sepsis measure, talk to us today about how our software can simplify this process for you and our experts can guide you through everything you need to know to succeed with this measure.
Sources
- Sepsis: https://www.mayoclinic.org/diseases-conditions/sepsis/symptoms-causes/syc-20351214
- Getting to Know Core Measure SEP-1: Early Management Bundle, Severe Sepsis/Septic Shock: http://www.providentedge.com/getting-know-core-measure-sep-1-early-management-bundle-severe-sepsisseptic-shock/
- CMS Webinar: Slide 9: https://www.qualityreportingcenter.com/wp content/uploads/2018/02/IQR_slides_Sepsis_v5.3a_20180227_vFINAL508.pdf
On-Demand Webinar:
Conquering Sepsis: Best Practices for Improvement
Is your organization struggling to successfully report on the sepsis measure and improve sepsis performance?
In this free educational webinar, you’ll hear from Beaufort Memorial Hospital whose sepsis journey began in 2006 and now has a sepsis performance of over 90%. We will share the specific actions Beaufort took to impact their performance and some best practices you can take back to your organization.
In this webinar you will:
- Learn how Beaufort Hospital improved their sepsis performance to its current 91% rate
- Understand the specific actions Beaufort took to impact their sepsis performance
- Hear tips and best practices for sepsis success


.png?width=352&name=2026%20Quality%20Reporting%20Deadlines%20Guide%20(1).png)



Comments