3 Ways to Prepare for the CMS Web Interface Retirement

By now, you have undoubtedly heard the good news: the sunsetting of the CMS Web Interface has been delayed until 2025. But don’t pop the champagne just yet.
The big switch may have slowed down temporarily, but there are still many questions your organization needs to answer—and significant processes you need to establish—over the next ~24 months. Here’s how to make the most of this breathing room period before the CMS Web Interface is officially retired.
Step 1: Map Out Your Data Aggregation Plan Now
Does your team understand exactly what the retirement of the CMS Web Interface means for your organization? If not, here’s a quick primer:
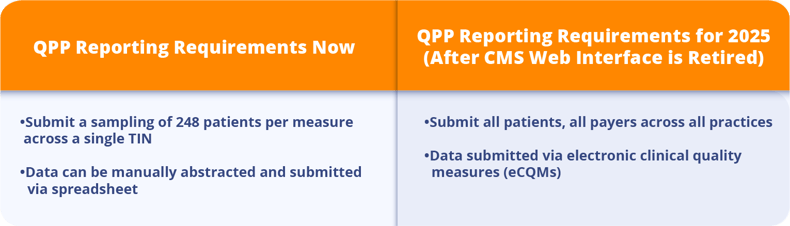
Since 2017, the Quality Payment Program (QPP) has allowed large organizations and ACOs to use the CMS Web Interface reporting method to complete MIPS requirements. This has allowed qualified organizations (those with >25 clinicians/NPIs) the option to report MIPS quality using a sampling of only 248 patients for each measure across a single TIN, selected through Medicare Part B claims. This small data set is typically abstracted into a spreadsheet, submitted, and that’s a wrap.
Now, in an effort to begin collecting more meaningful data, CMS has upped the ante in a big way. Once the CMS Web Interface is retired, ACOs will be required to report all quality measures on all patients and all payers across all practices for 365 days of the year using either eCQMs (electronic clinical quality measures) or CQMs (clinical quality measures). For most ACOs, using CQMs is impractical. That would be entirely too much abstraction to actually be feasible. That means eCQMs is the measure type all ACOs will likely need to use going forward.
ACOs must learn to juggle multiple, disparate EHRs and data collection methodologies. Developing a cohesive data aggregation system is going to be a major undertaking. Your senior leadership, quality management, and information technology teams need to start planning what that looks like for your ACO now.
Step 2: Choose Your ACO’s Reporting Framework
If you are a Medicare Shared Savings Program (MSSP) ACO, CMS is limiting you to just one reporting framework moving forward: the APM Performance Pathway, or APP.
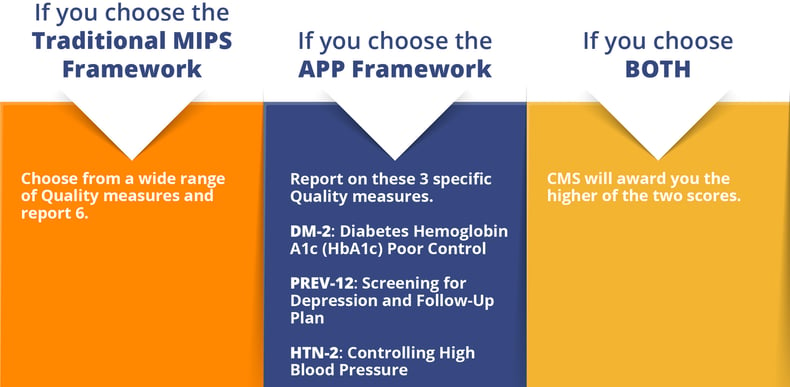
For all other ACOs you have 3 options to choose from: the APP framework, the traditional MIPS framework, or both. In our opinion, the APP framework is the obvious choice for 2 reasons:
- You only have to submit APP’s 3 required measures (versus MIPS’ 6 required measures out of 48 possible choices).
- Those 3 required measures tend to be less burdensome on practices on a practical, day-to-day workflow level.
- Generally these measures will be applicable to at least some of the clinicians in your group (see chart below for a list of the measures).
If you choose to submit under both frameworks, CMS will award you the higher of your two scores. Provided that you have a quality management vendor (like Medisolv) who handles your submissions for you, this may be a valuable option for your ACO, as it gives you an added layer of protection, while placing the bulk of the administrative burden on your vendor.
Here is a list of quality measures on the CMS website.
Step 3: Get to know your data landscape
The most important thing you can do right now is understand what your data landscape looks like. Here are a couple of questions you should know.
- Which practices are on which EMRs? Make a list.
- How many instances of each EMR vendor do you have?
- Do you have any practices still on paper charts? (<<if so you cannot report to CMS)
- How many practices are on less common EMRs?
- Can every single practice generate a QRDA I file (especially focus on those practices with less common EMRs)
- Do you capture CPT II (G codes) in a database for all practices?
This information will help you to choose whether you want to submit eCQMs or MIPS CQMs. It will also inform you as to wether or not you have to set up conversations with any practices not able to provide your group what you need.
Final Thoughts: What if CMS Pushes Its Deadlines Again?
Yes, it’s true. History has proven that CMS could change the rules and deadlines on us any minute, however, in the 2023 final rule CMS made it clear that they are still intending to sunset the CMS Web Interface Measures by 2025 for everyone.
It's in your best interest to start looking at your data through the all-patients, all-payers, all-practices lens now. It is the key to unlocking so many other patient care goals for you, including improving population health, reducing health care costs, and advancing health equity. For too long, the CMS Web Interface had made quality reporting a box that organizations had to check. It’s time now for organizations like yours to lead the charge to elevate the role of quality data in patient care. Together, we have the power to put quality data to good use.
More Resources to Prepare Your ACO for What’s Next
At Medisolv, we offer so much more than quality software and start-to-finish submissions management. We’re the quality improvement partner committed to deciphering and anticipating CMS’s regulatory changes for you—so that you can keep your organization ahead of the curve. Check out some of our additional resources now:
- dQMs: Preparing for the Unknown
- What is Social Determinants of Health (SDOH) Data?
- [e-Book]: CMS Web Interface Transition Guide
Medisolv Can HelpAlong with award-winning software, each client receives a dedicated Clinical Quality Advisor that helps you with your technical and clinical needs. We consistently hear from our clients that the biggest differentiator between Medisolv and other vendors is the level of one-of-one support. Especially if you use an EHR vendor right now, you’ll notice a huge difference.
|

.png?width=352&name=2026%20Quality%20Reporting%20Deadlines%20Guide%20(1).png)



Comments