Changes to 2020 MIPS Reporting Requirements
CMS changed the requirements for 2020 MIPS reporting due to the COVID-19 pandemic. Actually, it might be more accurate to say they are providing you with more flexibility in what you submit to the program for 2020.
Key takeaways:
- There is no blanket waiver for MIPS
- You may apply for a hardship for MIPS
- Depending on if you are approved, you may reweight your categories
What might be some issues with reporting MIPS in 2020?
Well it’s all messed up right? Let’s start with telehealth. There has been an explosion in telehealth services because of the pandemic. Many of the eCQMs in the Quality category of MIPS are outcomes based, like the Controlling High Blood Pressure Measure. Patients didn’t and still aren’t going into their primary care doctor’s office to get their tests completed and they don’t have a way to test at home. So, many of the measure results for the first half of the year are either super low or completely off. CMS did release new guidance on the allowance of telehealth encounters in eCQMs which may help some of this.
Also read: We Need a Better Way to Measure the Quality of Telehealth Services
Another issue is cost. Everything is canceled this year! All of these canceled elective surgeries are putting a financial strain on everybody. We are starting to see some fallout from these financial issues. Clinics are closing, hospitals are closing or going bankrupt and staff is being furloughed or laid off. The Cost category of MIPS this year will be messy at best.
There are hundreds of other issues that have come up because of COVID-19, and some may be specific to your exact situation. Perhaps you were in the middle of an EHR migration that was permanently put on hold. What a nightmare. How are you supposed to fulfill the Promoting Interoperability category requirements when data is everywhere and nowhere?
This year for MIPS you must achieve a minimum score of 45 points which will be difficult to achieve given how much is out of your control this year.
Ok, ok we are done panicking with you now. Let’s talk about what can be done and how you are going to make a decision as to what to do.
Applying for a 2020 MIPS hardship
The first thing to understand is that there is no blanket waiver for MIPS, so you have to do something this year. That something is applying for a hardship before December 31, 2020.
Clinicians who were significantly impacted by COVID-19 may submit an Extreme & Uncontrollable Circumstances Application to reweight any or all of the MIPS performance categories.
By applying for the hardship, you give yourself time to see what the effects are/have been on your clinicians. Once you have the exception approved, you can decide later what, if anything, you want to submit.
During the application process you will be able to select which categories you want reweighted. If approved, your selected categories will be reweighted to 0%.
So, if you ask CMS to reweight all categories to 0% and then later decide to submit Quality and Improvement Activity data, your data will be evaluated for those categories using the weighting below.
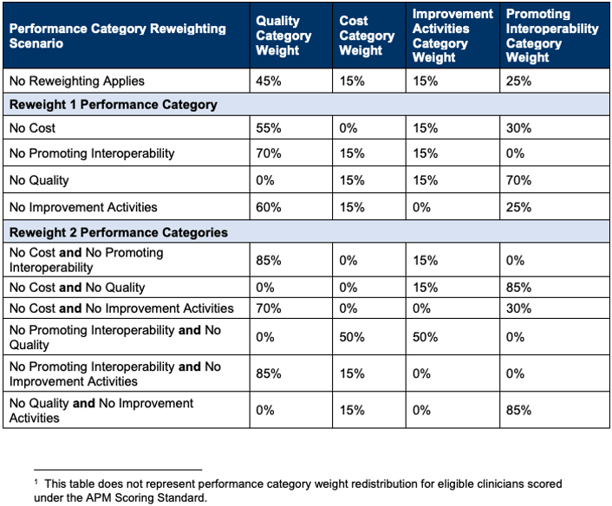
Now if you reweight more than two categories (which you can do but is not shown in the chart above) you will automatically get a score of 45 points and receive a neutral payment adjustment in the 2022 payment year. Basically, if you’re going to submit any data this year, submit at least two categories of data or submit nothing at all.
Medisolv clients will receive an update later this year that will allow them to see how their MIPS score is calculated in each of the scenarios listed in the chart above. This can help your team make informed decisions about your 2020 submission.
How to get approved for a 2020 MIPS hardship exception
Those requesting relief will need to provide a justification of how their practice is/was significantly impacted by the public health emergency. We take this to mean that CMS is going to be carefully considering each hardship application and only approving those cases where they feel there is some justification.
We suggest that you carefully look at how COVID-19 has affected your Eligible Clinicians.
Consider the following:
- Are you in an area that was classified as high-risk?
- Could you get your public health department to put together a letter saying your hospital was at high risk?
- Were a bunch of staff from other departments pulled into direct care positions?
- Did your financial hardship cause you to lay off or furlough staff?
- Were any technology implementations (critical to MIPS) delayed or canceled because of COVID-19?
What do you think you can get approved for? What truly impacted your ability to monitor and improve your clinician care this year?
Deciding what to submit to MIPS in 2020
Once you are approved, you have to decide what you will submit.
We suggest that you start with the Cost category. You should be receiving your 2019 Cost report from CMS mid-summer if you don’t have it already. Take a look at how you performed last year. Now compare that with the data you have this year. Has your overall practice revenue decreased due to telehealth being reimbursed at lower rates? Did you experience a loss of lab and procedure revenue? How about surgeries? The Cost measures involve OR procedures which may have a big impact on your overall performance in this category.
We think Cost might be a good category to ditch this year. It’s going to be a mess and likely not a very good representation of your clinicians.
The other one we think you might consider ditching is the Promoting Interoperability (PI) category. Did you have a lack of connectivity with the internet? Did you lack control over the availability of CEHRT? Did you have any issues with clinic closure, severe financial distress or vendor issues that would affect the PI measures? Lacking 2015 Edition CEHRT does not qualify as a reason to submit an application, but other variables that were out of your control might be a reason for the exception.
* Note There are certain clinicians who receive automatic reweighting in the PI category. Check the QPP Participation Status Lookup Tool for any special statuses assigned at the clinician level.
So that leaves the Quality and the Improvement Activities categories. Improvement Activities should be pretty straightforward, and you still have time to plan for this one. Review the measures available to you and make a plan for improvement for 90 days. Then document what you did as you go along. You can begin this project as late as October 2, 2020. Also remember that CMS added a new COVID-19 clinical trials improvement activity which would be counted as a high-weighted measure. But remember, at least 50% of your clinicians in the TIN must participate in the improvement activity.
And finally, the Quality category. The only change you should note here is that there is a maximum of 60 points in this category. Originally, CMS intended to include the All Cause Readmission measure (as they usually do) for any groups that include 15 or more clinicians. The All Cause Readmission measure is based on administrative claims data but only if there are 200 or more attributed hospitalizations. In previous years that would make your max score in this category 70 points, but CMS is not calculating that measure this year.
How to get help with MIPS in 2020
Of course, Medisolv is here to help you with your MIPS needs. Our MIPS software comes with our award-winning consultative services to help you make sense of this program. Request a demo to see our software in action and talk to someone about your specific situation.
CMS Resources
- QPP Exception Applications Fact Sheet
- QPP COVID-19 Response Fact Sheet
- Contact the Quality Payment Program at 1-866-288-8292, Monday through Friday, 8:00 AM - 8:00 PM ET or by e-mail at: QPP@cms.hhs.gov.
- Visit the Quality Payment Program website for other help and support information, to learn more about MIPS, and to check out the resources available in the Quality Payment Program Resource Library.

.png?width=352&name=2026%20Quality%20Reporting%20Deadlines%20Guide%20(1).png)



Comments