13 Highlights from the 2018 Quality Payment Program Proposed Rule

Last week, CMS dropped the proposed rule for the Quality Payment Program (QPP) in year two. Based on the new requirements proposed in this document, it's clear that CMS is attempting to provide relief to small practices that may be struggling and ease the transition into QPP for all clinicians.
We have pulled together the top 13 significant highlights from this proposed rule. Here’s what you might expect for MIPS in 2018.
In a statement from the executive summary, CMS said that “as the Quality Payment Program moves into the second year, CMS wants to ensure that there is meaningful measurement and the opportunity for improved patient outcomes while minimizing burden[s].”
The extensive proposed rule spans over 1,000 pages and the executive summary alone is 26 pages. Below, we touch on just the highlights of the proposed changes to the Quality Payment Program in 2018. Keep in mind that these are proposed changes. Nothing is set in stone. Is it ever with CMS?
1.Eligibility Requirements
Eligibility requirements will change to make it easier for clinicians to be exempt from MIPS reporting. If you billed Medicare less than $30,000 in allowable charges OR saw less than 100 Medicare Part B patients, you are excluded from MIPS in 2017. Next year, if you bill Medicare less than $90,000 in allowable charges OR see less than 200 Medicare Part B patients, you are excluded.
More details >>
2. EHR Technology
CMS did a good job of scaring everyone into thinking they had to be ready to use the 2015 Edition of Certified EHR Technology (CEHRT) in 2018. In the proposed rule, however, they have backed away from that requirement, now permitting Eligible Clinicians to still use the 2014 Edition instead. While it’s no longer a requirement, CMS is encouraging the use of 2015 CEHRT with a nice bonus for those who do use the 2015 Edition.
3. Help for Small Practices
Small Practices get several breaks in this upcoming year, including the following:
a. Five bonus points added to their MIPS final score;
b. New hardship exceptions in the Advancing Care Information category;
c. Continuing to award small practices three points for Quality measures that don’t meet the Data Completeness requirement;
d. And increasing the low-volume threshold so that more small practices are exempt from MIPS.
4. Reporting Options
No longer can you “Pick Your Pace” for reporting to MIPS. For the Quality and Cost categories you must submit 365 days of data. For the Improvement Activities (IA) and Advancing Care Information (ACI) categories you must submit 90 days of data.
5. MIPS Score Weighting
The categories are weighted the same as 2017. They had originally indicated they would add the Cost category to the final score, but in the proposed rule, they are not calculating cost as a part of the MIPS final score. Here are the proposed category weightings for 2018.
a. Quality = 60% of total score
b. Improvement Activities = 15% of total score
c. Advancing Care Information = 25% of total score
d. Cost = 0% of total score
6. Category Requirements
The measure requirements for the Quality, IA and ACI categories do not change, but they did propose to modify and add several measures in each category.
More details >> (Pages 8 - 16)
7. Submission Method
Last year, you had to choose one submission method per MIPS category. This year, you can use multiple submission methods for each MIPS category.
8. Performance Threshold
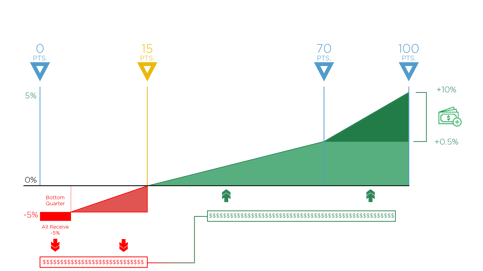 You must achieve at least 15 points to avoid the -5% penalty in 2018. That’s up from the three-point minimum of 2017. On the right, you’ll see a graph displaying the performance threshold minimum at 15 points and the performance threshold for exceptional performance at 70 points. Once you hit that 70-point threshold you will earn bonus money on top of any money you make from scoring above the 15-point threshold score.
You must achieve at least 15 points to avoid the -5% penalty in 2018. That’s up from the three-point minimum of 2017. On the right, you’ll see a graph displaying the performance threshold minimum at 15 points and the performance threshold for exceptional performance at 70 points. Once you hit that 70-point threshold you will earn bonus money on top of any money you make from scoring above the 15-point threshold score.
More details >> (Pages 17 - 18)
Also see: How Can I Make Money in the First Year of MIPS?
9. Payment Possibilities
And speaking of money, you can get up to 5% added to your Medicare reimbursement funds by performing well in MIPS next year. Conversely, you can expect to receive a -5% reduction to your Medicare reimbursement funds if you don’t meet that 15-point performance threshold score.
10. Facility-Based Scoring
CMS proposed to add a voluntary, facility-based scoring option in 2018. Any facility-based clinicians who have at least 75% of Medicare services supplied in the inpatient hospital setting can convert their hospital’s Total Performance Score into a MIPS Quality and Cost category score.
11. Virtual Groups
CMS is creating Virtual Groups, which will allow individual clinicians and small groups to come together to form one virtual group which can report together. Clinicians do not need to be in the same area of the country or be in a similar specialty to be in the same group.
12. Improvement Bonus
Clinicians will be rewarded if they demonstrate any improvement to their 2018 Quality category performance compared to their 2017 performance.
13. Complex Cases Bonus
For clinicians who work with patients that have more complex cases, CMS will award up to three bonus points to the clinician’s MIPS final score.
And those are the highlights. As we wait for the final rule to drop, start thinking about what you can do now to make it easier for your clinicians to perform their best in 2018. We also encourage you to join the conversation. CMS is accepting comments on the proposed rule until 5 p.m. of August 21st, 2017.
[E-BoOK]
Beginner's Guide to MIPS Year 2
With the MIPS final rule in place, providers nationwide are trying to understand the changes for the year to come. MIPS offers unprecedented opportunities to substantially increase payments for exceptional performance.
Medisolv has the tools you need now to prepare. This FREE 31-page eBook is a beginner’s guide to the MIPS program Year 2. You'll learn about the basics of the Quality Payment Program under MIPS in 2018.
This guide includes:

.png?width=352&name=2026%20Quality%20Reporting%20Deadlines%20Guide%20(1).png)



Comments