How to read an eCQM specification
Hospital eCQM specifications are meant for computers not humans. And yet, it’s up to you as a human (I mean, I assume you’re a human reading this) to interpret this computer document and translate that into something that generates valid eCQM performance results.
This article walks you through how to read a hospital eCQM specification. Let’s go!
What are eCQMs?
eCQM is an acronym that stands for Electronic Clinical Quality Measure. You may already be familiar with Clinical Quality Measures or CQMs since those have been around for some time. For many years, quality teams have abstracted these core measures to evaluate the quality of care your clinicians are providing to your patients.
eCQMs operate under the same premise but the catch is that in order for an eCQM to be captured, every element that makes up that measure must be documented electronically in your EHR. Nothing can be documented on paper or in a dictated note.
Like core measures, eCQMs were created to improve the quality of care in a hospital setting. When eCQMs first came on the scene it was in conjunction with the Meaningful Use initiative also known as the EHR Incentive Program. Hospitals were encouraged with monetary rewards for getting their hospitals electronically up and running.
The end goal for CMS is to have hospitals use their eCQM results (which pull data directly from their EHR) to improve the quality of care they provide their patients.
eCQMs, much like core measures, follow an algorithm to assess whether or not a patient has successfully met the measure requirements. eCQMs use something called a specification which contains the logic that is used to assess whether the patient has successfully met the measure requirements.
How does an eCQM work?
Each eCQM has an associated specification (spec). These specifications are created and owned by different organizations such as the National Quality Forum, The Joint Commission (TJC) or even Medisolv. All of the specifications can be found on the TJC or CMS website or on the eCQI resource center. Or if you are a Medisolv client, our software provides specs to you within the product, so you don’t have to search for them online.
That spec outlines all of the data requirements in order to meet the measure. Clinicians then document the data in a structured field in your EHR. Each documentation field (for the most part) is mapped to codes. That is the key difference between these measures and the chart-abstracted measures. The codes will drive your eCQM results. If you don’t have a code mapped to those documentation fields, you won’t get any results.
How to calculate an eCQM measure performance rate
Each eCQM specification defines the populations that a patient will qualify for. That means depending upon certain factors (such as demographics and fulfillment of care) a patient moves through the populations until they reach their final “bucket.”
The population buckets are:
- Initial Population
- Denominator
- Denominator Exclusions
- Numerator
- Numerator Exclusions
- Denominator Exceptions
In most cases the Numerator means the patient’s treatment was in alignment with clinical protocols. But for inverse measures, Numerator means treatment did not align with protocols and/or outcomes were unexpected.
Your performance rate is calculated by dividing the Numerator by the Denominator minus any Exclusions and Exceptions. Multiply that by 100 to get the performance percentage rate.
Let’s say you had 100 patients make it to the Denominator population and 20 of them fell into the Denominator Exclusion population. Then you had 60 patients qualify for the Numerator. You would take your 100 patients and subtract 20. You would then divide the 60 patients in the Numerator by the 80 patients in the Denominator population to calculate your performance rate, which for this example would be 75 percent.
How to read an eCQM specification
Let’s use a specification example to walk through each part of the spec.
We will use the measure example STK-2, Discharged on Antithrombotic Therapy. Click here for the spec sheet.
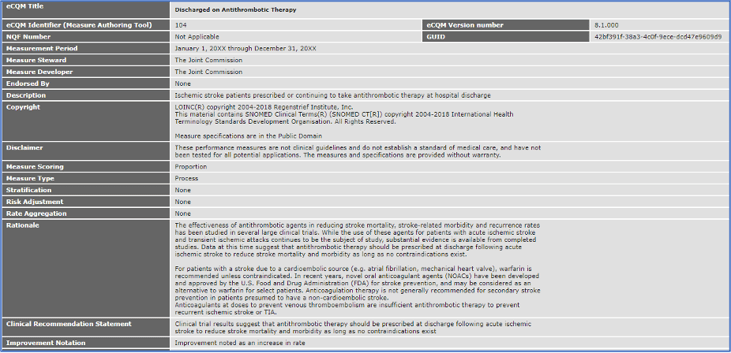
At the top of the spec is the basic information associated with each measure such as the name, the measurement period, the measure steward, developer and endorsement.
I want to draw your attention to the section labeled rationale. This rationale statement is really the intent of the measure. It attempts to give you the reason behind why this measure should be captured and improved upon. This is helpful for educating clinicians and stakeholders.
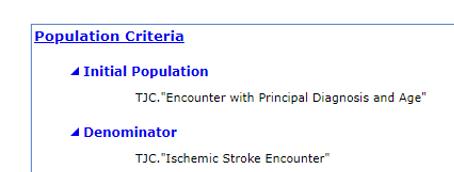
As we scroll down the spec sheet, we come upon the population criteria for the spec. In this section a series of statements define which population a patient would fall into. Keep in mind, these descriptions do not tell the whole story, there’s a lot more you have to do to make sure patients qualify correctly.
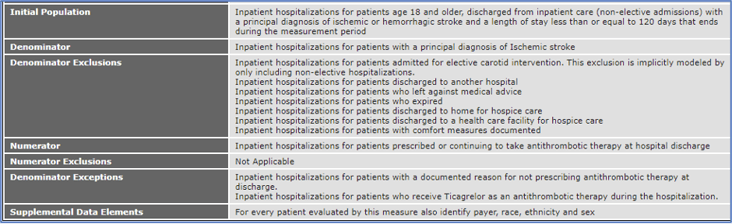
The next sections of the specification provide the details you need to understand how patients meet the population requirements. I am going to walk you through how to understand what’s needed for a patient to qualify for each of these populations.
The first section is called the Population Criteria. It’s a high-level summary of the data elements a patient must have electronically documented to meet the populations. For example, the Denominator criteria simply explains that a patient gets to this population by having an “Ischemic Stroke Encounter.”
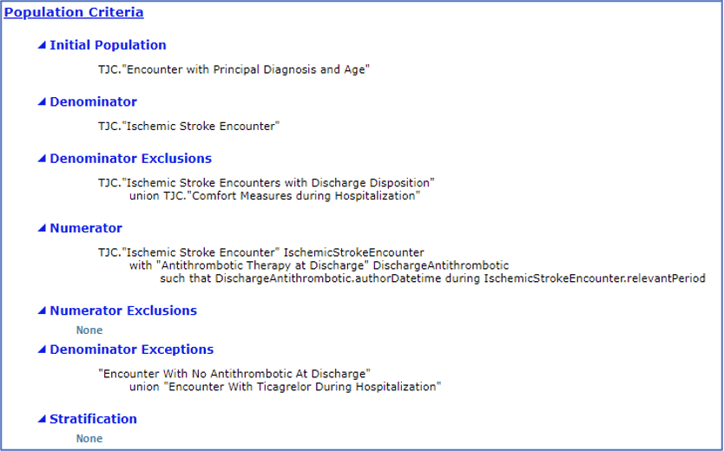
So, while it provides a short description the population , you need a more detailed definition in order to fully understand what each statement means. That’s what you’ll find as you scroll to the Definitions section below.
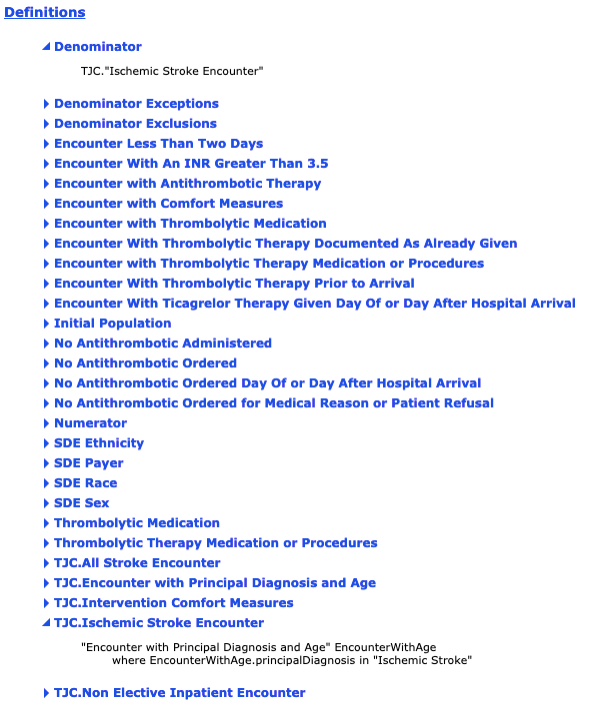
This is where it gets downright tricky. In the definition section, you will find every statement from the population criteria section above. Each statement has a corresponding definition that may include additional logic and additional definitions.
You read that right, there are definitions for the definitions!
In order to view and understand all of the definitions, you have to do lots (and lots) of scrolling. It can be a very long process to look through each statement and make sure you fully understand exactly what makes up each population but the definitions, logic statements and additional details are what truly define the population requirements and measure evaluation steps.
Let’s look at the example and try to connect the dots:
Step 1: Note that in the Population Criteria section the Denominator is “TJC.Ischemic Stroke Encounter.”
Seems clear enough right? Wrong.
Step 2: Remember when we mentioned scrolling? Do that now until you get to the Definitions section and find the Denominator definition.
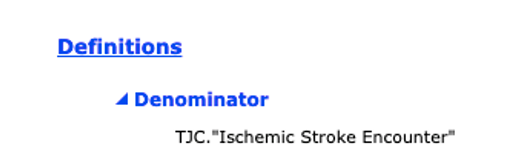
Not at all helpful right? It says the same thing as the Population Criteria.
Step 3: Can you guess what we need to do now? Yup, scroll again to look for the definition of TJC.Ischemic Stroke Encounter.
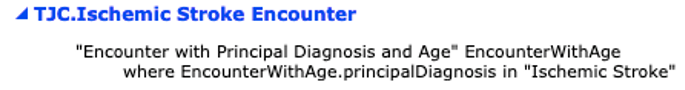
Ah! Finally, more information but guess what? Each of those statements are further defined in the same section.
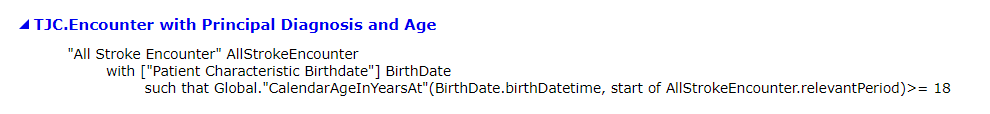
Step 4: Scroll some more to identify the definition of “Encounter with Principal Diagnosis and Age.” And again, more definitions of definitions are needed.
We could do this all day but I think you get the picture.
You must do this process for each population until you fully understand the patient population buckets.
Mapping a hospital eCQM
Once you understand the logic of the spec and how patients qualify for each of the populations, it’s time to consider how these populations are mapped in your system.
Scroll to the Terminology and Data Criteria sections. You’ll see a list of every data element that require mapping to codes in your in your EHR documentation. Every one of those elements you see listed needs to be mapped in order for the data to be evaluated and for your results to populate accurately.
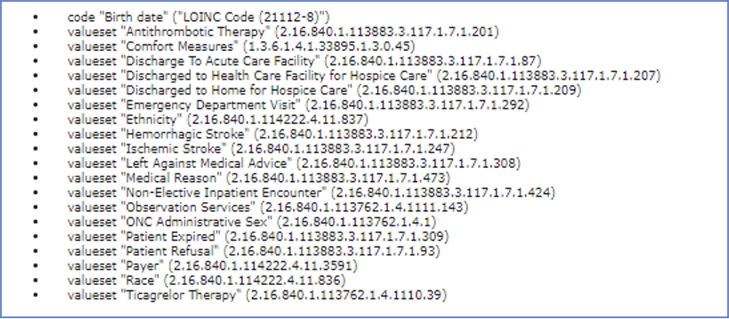
I keep talking about mapping these elements to your EHR using codes but where do you find out which codes you can use to map these elements? Well, if you look at the end of each data element, you’ll see a very long number. This is called an OID (object identifier) code. This is the number you will need to search for the appropriate codes.
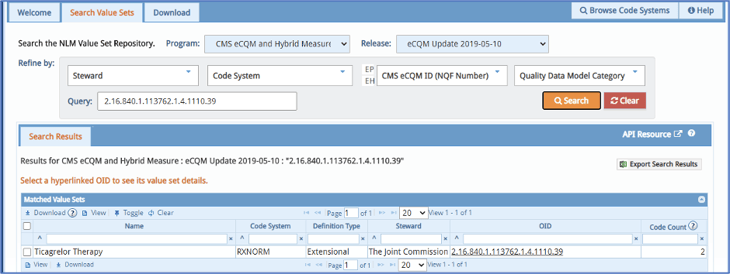
You must take that code and place it in the search box on the Value Set Authority Center or VSAC website. You must first have a login to VSAC before you can look up these codes.
Once in the VSAC website you input this OID code and up pops a list of all of the codes that can be used to map that particular data element within your EHR.
Be sure to select the correct program and release date at the top.
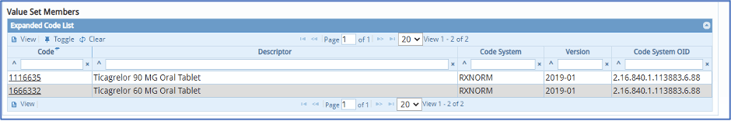
Some data elements like this one here have only a few codes and they all must be mapped in your system. Others have a list of hundreds of codes, and you have to decide which codes work best for your hospital.
In this example, you may already have documentation captured by clinicians in your EHR for this medication. In that case, all you need to do is map these codes to that documentation in your EHR and you’ve taken care of that element.
On the other hand, you may have to build out alternative documentation for your clinicians.
It’s that level of detail that you must get to in order to be successful with your eCQMs. Otherwise, your eCQM results will likely be inaccurate. That could mean your clinicians are caring for the patients properly but it’s not being reflected in the eCQM data due to a mapping error that could easily be fixed. And remember that your eCQM performance is publicly reported on the CMS Care Compare website in 2021 and beyond.
Annual eCQM specification updates
The last thing I want to mention is about specification updates. Each year CMS releases new eCQM specifications. You must look at the updates every year and see what has changed. You then must prepare to make the changes within your EHR system, but not before you have submitted your eCQMs for the previous year to the regulatory programs otherwise your eCQM data may be impacted.
Ideally, your hospital will submit eCQMs to IQR and CMS as early as possible in the year, allowing plenty of time for the team to review the specification updates in the fall of the preceding year and plan for any changes that need to be made in your EHR – this includes mapping, building and compliance training. That way you can switch over to the new version of the specifications as close to the start of the new year as possible (providing your vendor is ready) and evaluate your eCQM performance with as little disruption as possible.
To read more about the eCQM annual cycle read our post New eCQM Goals for the New Year.
Stay Ahead of the Quality CurveMedisolv Can Help
Here are some resources to help you get started:
|






Comments