How to Implement the Hybrid Readmission Measure

Did you know that a liger is a real animal? No kidding. It’s a male lion and a female tiger; thus, a liger. When I find myself trying to explain the hybrid readmission measure, I often begin by telling people it’s like a liger. It’s a combination of two different things that have been around for a while but have formed to create a brand-new thing.
Don’t judge how my brain works.
A hybrid measure combines claims data and electronic data from your EHR; thus, creating a hybrid measure.
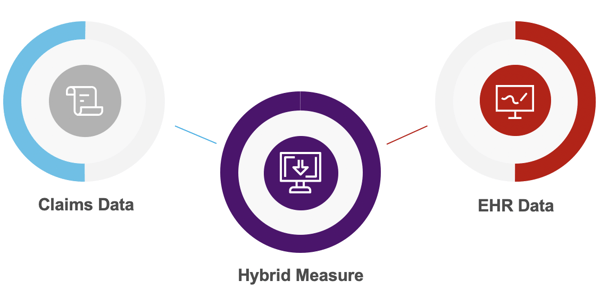
To be successful at capturing the hybrid measures you need to be successful at capturing both of those key data sources.
Claims data you’ve been doing for a long time (submitted to bill insurance companies for the patients’ visits). No big deal. The key here is that the claims data must be linked with all of the EHR data (all of the data captured electronically during a patient’s visit).
Ok, let me take a step back. Why are we even doing this in the first place?
Why do we need hybrid measures?
Here’s a summary of the reasons CMS is moving toward hybrid measures.
Preference: Clinicians have been talking about this for years. They believe that using clinical data to assess a hospital’s performance makes more sense than just straight billing.
Duh, yes. Somebody give CMS a cookie for listening.
Data collection: That transition from paper to EHR creates an opportunity to integrate clinical information into hospital quality measurement without the burden of manual chart abstraction.
Accuracy: This is a biggie. The data we get from claims does not contain any risk factors associated with severity, which can really impact these calculations. The best-performing risk adjustment models typically include risk factors that assess both comorbidities and severity. Historically, the claims-based models do assess the comorbidities, but the electronic clinical data provides the measure of severity when the patient is admitted.
That’s why these hybrid measures are important for you. It’s not just one more thing to do. This should hopefully be a good thing.
How does CMS calculate the Hybrid Hospital-Wide 30-Day Readmission Measure?
This measure calculates a hospital’s Hybrid Risk-Standardized Readmission Rate. The calculation is complicated to explain. It incorporates a lot of different things to provide hospitals with their performance.
So, here’s a cringe-worthy simplification of the math created by a lot of smart people.
The rate is calculated by:
- Using unplanned readmissions within 30 days from index admission
- Combining claims and EHR data
- Adjusting for differences in case mix and service mix across all hospitals
The goal in this is:
- To identify the critically ill patients that have a higher probability for readmission and take that into account when calculating this rate.
How and when do we submit the hybrid readmission measure?
By 2023 the Hybrid Hospital-Wide 30-Day Readmission (HWR) measure will be required as a part of your IQR requirements. There are two years of voluntary submission proceeding that requirement.
| Voluntary Measurement Period |
| July 1, 2021 – June 30, 2022 |
| July 1, 2022 – June 30, 2023 |
| Mandatory Measurement Period |
| July 1, 2023 – June 30, 2024 |
| Results Posted to Hospital Compare |
| July 2025 |
Hospitals must submit certain data elements from a patient’s electronic record and submit to CMS using a QRDA file.
Does this sound familiar?
It’s very similar to what you do for eCQM submissions right now. In fact, there is a specification for this measure and it looks like an eCQM spec. The logic is in the same format but it’s not technically a measure specification. Think of it more as a guide.
Either CMS was trying to make it easy on us or was trying to mess with us.
What is needed to capture the hybrid readmission measure?
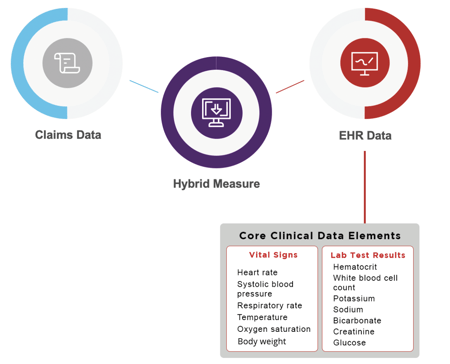
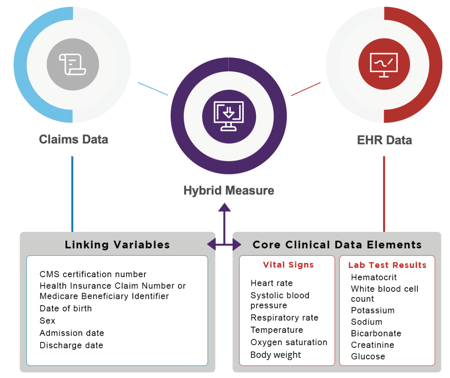
You need one more acronym definition here to understand this measure. CCDE stands for Core Clinical Data Element. These are the items you need to map in your EHR and include in your QRDA file to CMS.
Let’s look at what you need from your EHR and from your claims data.
What EHR data is used?
The 13 CCDE that you must submit in the QRDA file are in two buckets: vital signs and labs.
What claims data is used?
These linking variables need to be included in the QRDA file that you submit to CMS. If they can’t connect the two then they won’t be able to calculate the measure.
Implementing the hybrid readmission measure
Alright, are you ready? Let’s walk through the specification together and then explain the process of implementation and mapping.
Here’s the specification: https://www.qualitynet.org/inpatient/measures/hybrid/methodology
Download this and keep it at your fingertips. Clients: You have this available in the product when you click on the hybrid tab.
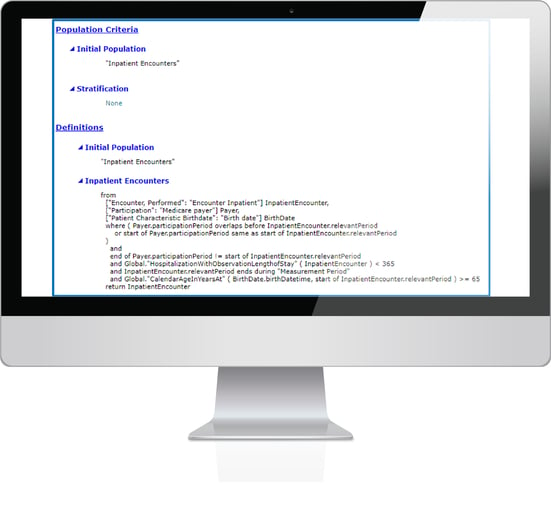
The spec can look completely overwhelming when you first look at it. But it’s not that difficult to understand once you know what you’re looking at.
Let’s break this down into manageable sections.
Identifying the population
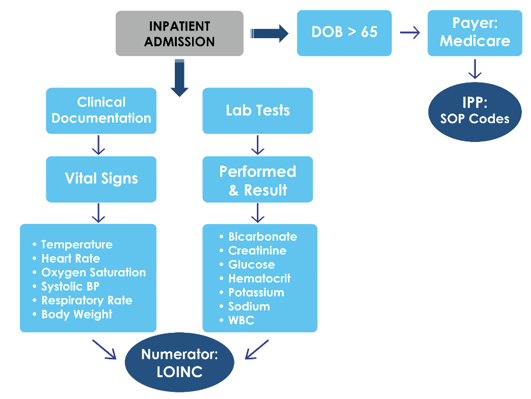
The Initial Population is all inpatients that are 65 or older who have Medicare as their payer. They will be excluded if there is a planned readmission, psychiatric diagnosis or cancer treatment. That’s what this section of the specification says.
Understanding the logic
Alright, now let’s move onto the logic section.
This is telling you that it’s looking for the earliest instance of at least one of the 13 core clinical data elements within specific time frames.
Let’s move to the “Functions” section of the spec to understand the timing requirement better.
Below is a picture of the “Functions” part of the specification which tells you the specific timing of the CCDE.
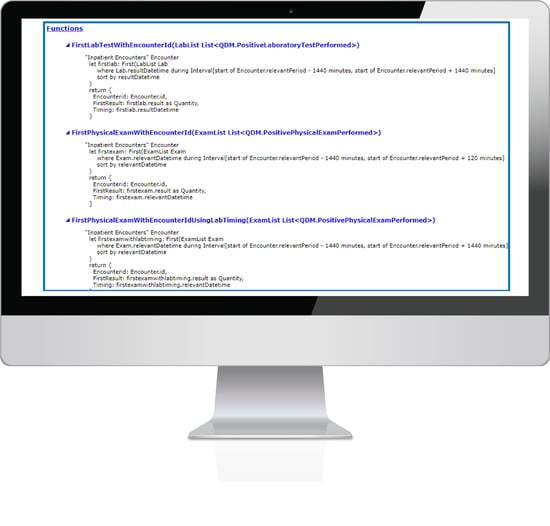
Supposedly this explains how the timing works for each of these elements. But honestly, it’s such a technical jumble. I’ll explain it simpler below.
In a nutshell, this measure will capture the first instance of documentation.

This means the earliest instance of documentation that meets the timing requirements above will be evaluated and included in the QRDA file.
The measure will look back to find these core clinical data elements 24 hours before the patient becomes an inpatient. It will also look for any labs and weights captured 24 hours after admission as an inpatient. And it will also look for vital signs captured two hours after admission.
Put simply, you’ve got to capture all 13 CCDE within these narrow time frames or it will not be included in the QRDA file you send to CMS. And remember, those CCDE are telling CMS how sick your patients are and adjusting your readmission rate based on that information.
Data Elements
Alright, remember when we looked at which core clinical data elements are used from your EHR at the top of this article? That is what you are seeing listed here in the data elements portion of the specification.
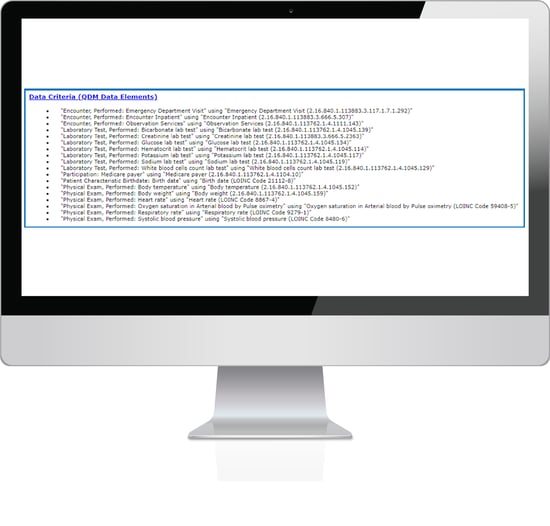
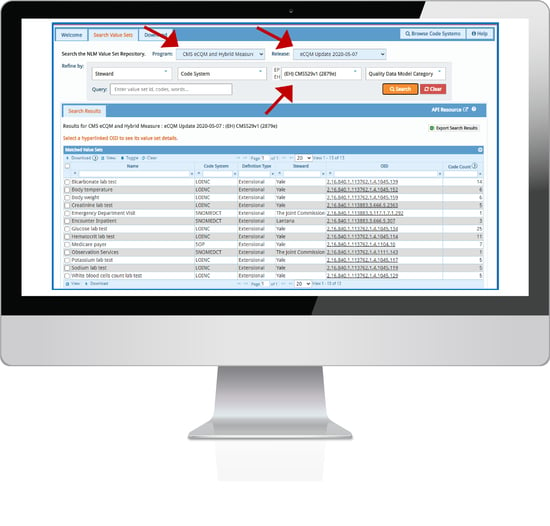
The data elements listed here are the ones you must map in your EHR in order to properly capture the measure. To the right of each of these elements is a long string of numbers. This is the OID (Object Identifier Code). This is the number you put into the Value Set Authority Center website to look up the value sets to map to your system.
Clients: you can just use the value set search tool in our software.
Implementing the measure
Essentially, you must take all the data elements listed in the specification and map the value set codes to the places you document those elements in your EHR system.
Why don’t I organize this in a different way for you?
This is the hybrid measure workflow and I think it simplifies what you need to do here.
Ask yourself, where are you documenting all these elements in your EHR? Compile a thorough list.
When we first started working on implementing this measure with our clients, we found that we would be getting some of the documentation but not all of it. It turns out there was additional documentation being done in the Emergency room, or the Operating Room. We had to go back and figure out where all of these elements were being captured in their EHR. This goes back to timing. Think through all the locations where these elements are captured 24 hours prior to and 24 hours after admission as an inpatient.
Map the hybrid readmission measure
This list you’ve created that contains all the places where these CCDE are captured is also your list of what needs mapped in your system.
Once you have your list, go to the VSAC website, use the OID (long number at the end of the data elements section of the spec) to look up the value set. That will give you a list of all of the codes associated with that value set. This screenshot below shows you the value sets that need selected for this hybrid measure.
Note the arrows I put on here. These are the selections to make if you want to get this list. Clients: remember to use the the value set search tool in the software.
Review this list and figure out which of the codes from that value set needs to be mapped to the documentation and the labs and verify all of that is done accurately.
Again, you must map ALL of the places where these items are documented throughout your hospital system.
Monitoring and improving your hybrid readmission measure results
Once you think you’ve got this all set up and implemented, there comes the real test. You must have a way of going into your system and reviewing to see if you are really getting all of the elements captured.
See the tough part about this measure is that you won’t know your performance until CMS compiles the whole thing for you. But you sure as heck know that you don’t want to have a lower score because of something stupid like forgetting to map your blood pressure documentation.
At Medisolv…
Shameless plug
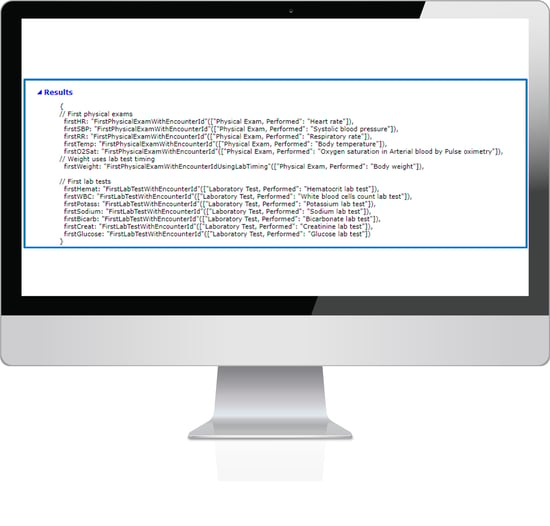
we have a CCDE missing results page for our clients. This shows you what elements are missing before you get to the submission phase. It looks like this.
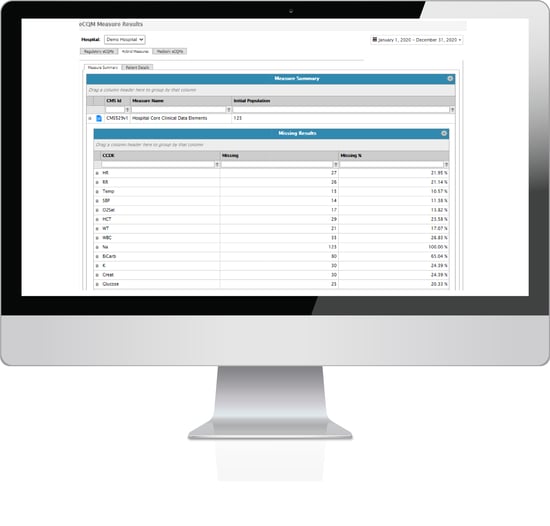
Even if you don’t use Medisolv, you should have a way of reviewing this data to ensure you aren’t making a mistake that is easily identified and fixed.
Well that’s it. You probably need to reread this article 10 times to get it, but you’ll figure it out. Good luck and call us if you need help!
|
Here are some resources that might be helpful:
|

.png?width=352&name=2026%20Quality%20Reporting%20Deadlines%20Guide%20(1).png)



Comments