How to Implement the Safe use of Opioids eCQM (CMS 506)
CMS released a new eCQM in 2020, CMS 506: Safe use of Opioids - Concurrent Prescribing. This measure is available to submit as part of your 2021 Inpatient Quality Reporting (IQR) requirements. By 2022, your hospital is required to report your performance on this measure for three quarters of the year.
It’s important you start tracking and improving this performance now since not only will this measure be required for submission soon, it will also be publicly reported.
What is CMS 506?
The purpose of the Safe Use of Opioids eCQM is to identify patients prescribed, or continued on, two or more opioids or an opioid and a benzodiazepine concurrently at discharge from a hospital.
This measure was actually based on a measure implemented by the Veteran’s Health Administration’s Opioid Safety Initiative and was associated with a 20% decrease in concurrent prescribing.
Why do we need CMS 506?
Did you know that concurrent use of benzodiazepines with opioids was prevalent in 31-51% of fatal overdoses? The rates of fatal overdose are ten times higher in patients who are co-dispensed opioid analgesics and benzodiazepines.
Another mind-blowing statistic is that more than half of patients who received an opioid prescription had filled another opioid prescription within the previous 30 days.
Studies have shown that eliminating concurrent use potentially reduces the risk of opioid overdose-related hospital visits, preventable mortality and costs associated with adverse events related to opioid use.
Opioid eCQM Requirements
Before we dive into the measure specification here is a quick review of the opioid eCQM requirements for 2021 and 2022.
2021:
- 2 self-selected quarters
- 4 self-selected eCQMs
Safe Use of Opioids eCQM: Available to submit but not required
2022:
- 3 self-selected quarters
- 3 self-selected eCQMs AND
- 1 Safe Use of Opioids eCQM
Safe Use of Opioids eCQM: Required for successful completion of the program
Opioid eCQM Specification
The process of implementing any eCQM always begins with a review of the specification.
Here is a link to the specification: https://ecqi.healthit.gov/sites/default/files/ecqm/measures/CMS506v3.html
Scroll to the bottom of the specification and read through the populations and the data elements required.
It’s important that everyone on your eCQM team understands the measure. It’s the same type of specification as every other eCQM you have. Familiarize yourself with all of the different segments of the measure logic. They clearly (or rather unclearly) explain what each of these different segments of logic mean. Below is a snapshot of the populations logic.
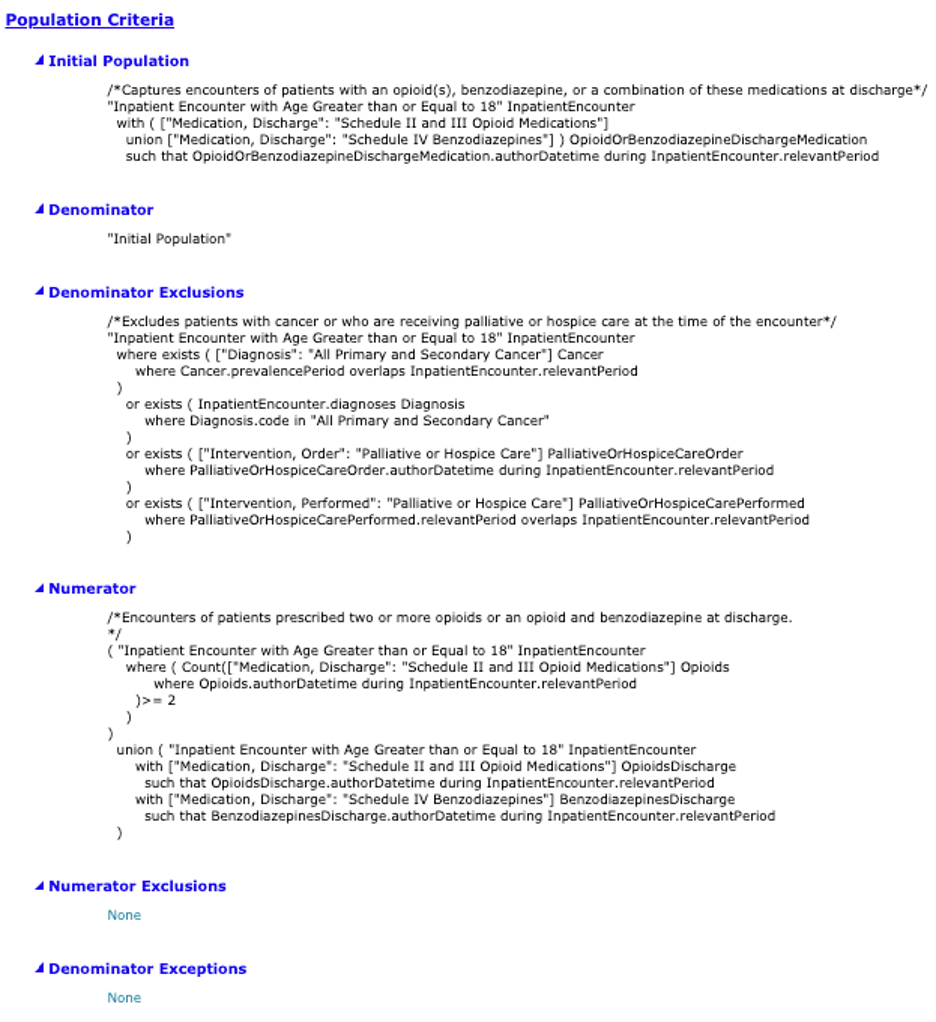
This screenshot is just a portion of the specification. It’s important that your team go through the spec line by line to make sure you really understand what it is saying. That means reviewing not just the section above but also the population definitions.
To keep us moving, I’ve simplified it below, but this won’t take the place of the thorough analysis your team should do.
INVERSE MEASURE
IPP / Denominator (What puts a patient into the IPP/Denominator?)
• Inpatient Encounter including Observation
• > 18 years of age
• Length of stay < 120 days
• Opioid or Benzodiazepine at Discharge
Denominator Exclusions (What excludes a patient from the Denominator?)
• Hospice or Palliative Care
• Primary or Secondary Cancer Diagnosis
Numerator (What puts a patient into the Numerator?)
• Two or More Concurrent Opioids at Discharge
or
• Concurrent Opioid and Benzodiazepine at Discharge
Denominator Exceptions
• None
The first thing to note is that this measure is an inverse measure which means a lower performance rate is better. As we go through the measure below remember that a numerator is actually bad in this case. The lower the numerator the better.
CMS has previously said they know it’s probably impossible to have a 0% performance rate because there are times when it is medically necessary to prescribe both medications. Instead, they expect you to be working on improving the rate to keep it as low as possible.
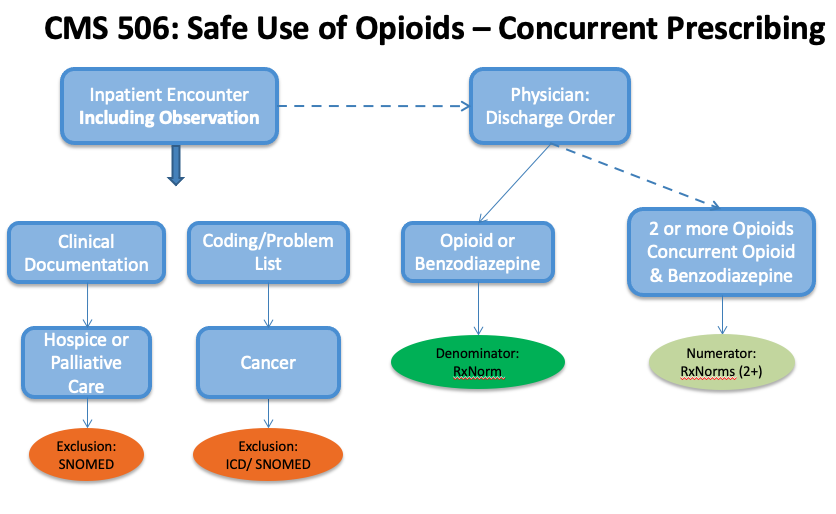
Opioid eCQM Workflow
Once your team feels comfortable with the specification, it’s time to figure out how you will set it up in your EHR.
Go back to your specification and scroll to the Data Criteria section. This section lists all of the data elements that need collected to properly capture this measure. Some of these may already be captured in your EHR.
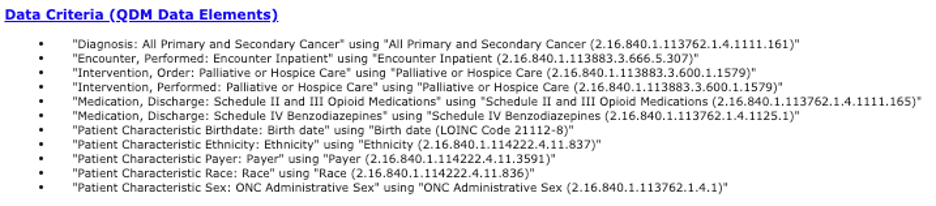
Your job is to figure out where your hospital currently captures each of those data elements. Are these already being captured in your system? If so, who does the documentation and where is it captured? Will you need to change or add any clinical workflows? If so, what?
Don’t make decisions that affect clinicians in a vacuum. Get your stakeholders involved including clinicians to make these decisions.
The workflow below visually explains how to capture and map data for this measure. Note how the workflow outlines all of the data elements listed in the Data Criteria section of the spec. You are responsible for making sure each of these elements are being captured in your system.
Map the Opioid eCQM
Once you decided how to best capture the measure in your EHR, then it’s time to map this measure to your system.
Go back to the Data Criteria section again. At the end of each data element bullet you’ll see a long string of numbers. This is called the OID (Object Identifier) code.

Take that code and type it into the Value Set Authority Center (VSAC) website. You’ll receive a list of value sets which will give you all of the codes you can map to your system. To help you with planning I have created this chart for you (below) which highlights the new value sets that you will absolutely have to map to your system in order to capture this measure.
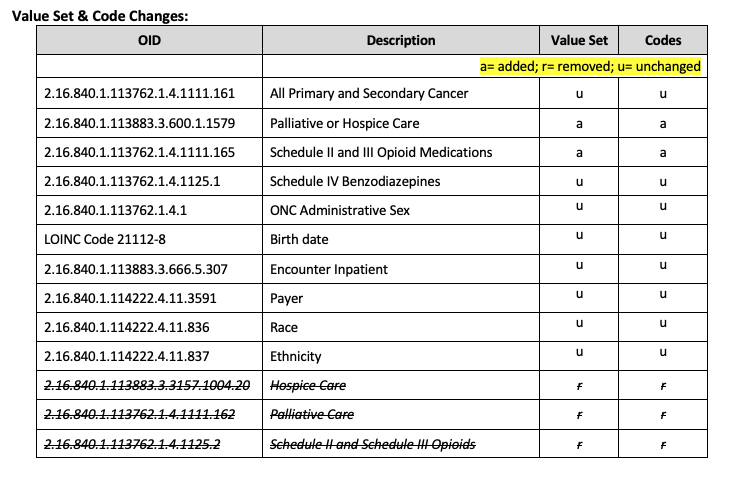
In the list above you can see that the first five OIDs are actually brand new to eCQMs. That means you will have to do some work to get these ones mapped even if you already capture all of the other eCQMs. After you’ve looked up the codes on VSAC, you’ll need to decide which codes and descriptions align with your current method of documentation. That’s what you did in the workflow analysis step.
Monitor and Improve the Opioid eCQM
After you have reviewed your workflow, identified any gaps, implemented workflow changes, added any required EHR builds and put the mapping in place, then you are ready to go live.
Use whatever reporting tool you have in place (like Medisolv's software) to start reviewing your results.
The more you look at your opioid eCQM performance the better. It gives you time to provide feedback, either technically or clinically, so you can achieve your best results.
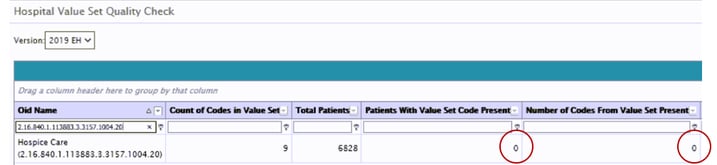
Start by making sure you are getting data into your report from all of the value sets in the measure. Go in, check your results and confirm you are seeing data populate for each of these elements.
The image below is one of the reports our clients have that shows you if the codes from the value sets are populating the eCQM reports. You can see there are nine counts of codes in the value set and zero patients and codes from the value set present. This indicates that none of the codes from the value set are coming into the reports; the mapping, workflow and/or technical set-up needs to be reviewed and corrected.
After you confirm that all data is populating the reports correctly then it’s time to evaluate the patients that qualified for the numerator. Remember, for this measure, the smaller the numerator, the better. Review all numerator patients to get additional details and then discuss potential resolutions with your eCQM team. This may involve education, changes in clinical documentation workflow, or the clinician may inform you that the concurrent prescriptions were medically necessary.
The last thing I want to mention is how important it is to involve your clinicians in this process. IT and Quality have worked together on eCQMs for a few years now. It’s important to include the clinicians too so the feedback loop is complete.
Here are some best practices we’ve gathered with our clients.
- Meet with the eCQM stakeholder team (include clinicians)
- Understand numerator qualifiers (what are the reasons why patients would be prescribed two opioid measures?)
- Plan for addressing gaps
- Plan for minimizing concurrent prescribing
- Education for all parties
- Ask for feedback and suggestions (especially from clinicians!)
I encourage you to set up the opioid eCQM now. Remember that in 2022 you need to start reporting on this measure. Whatever your performance is at that time will be what the public sees. Don’t do your reputation a disservice by having technical errors in your data. Start today and monitor and improve often, so that the 2022 submission data is an accurate reflection of the care your hospital provides!
|

.png?width=352&name=2026%20Quality%20Reporting%20Deadlines%20Guide%20(1).png)



Comments