How to succeed in the MIPS Improvement Activities Category

We are finishing up our three-part MIPS series in which we dig deep into each reporting category of MIPS. We offer tips to succeed and explore ways to identify the nuances of each category.
In this final part of our series, we explore the Improvement Activities category of MIPS, which is a brand new reporting category. The other MIPS categories all replace a former CMS reporting program. This category does not.
Of all the MIPS category requirements for 2017 submission, the Improvement Activities category might be the simplest.
The measures are not narrowly defined so you have a bit more room for interpretation. This flexibility allows clinicians the ability to make the measure work that has meaning for them, their staff or their patients.
If you haven’t had a chance to read the other deep dive blogs, check out the links below.
Also see: MIPS Quality – It’s All About the Numbers
Also see: A Deep Dive into MIPS: Advancing Care Information
Improvement Activities Reporting Requirements
This category of MIPS is focused on rewarding innovation and improvement activities that center around things such as care coordination, engaging beneficiaries, patient safety, expanding patient access and population management. In 2017, the Improvement Activities category is worth 15% of your total MIPS score.
Also see: The Four Pillars of MIPS Reporting (category score breakdown)
There are 92 activity options for you to choose from. These activities revolve around providing a patient-centered approach to improve your clinical practice or your care delivery.
You must report up to four measures to equal a score of 40 points to earn full credit for this category. You also must report each measure with data documenting that the activity was done for a minimum of 90 consecutive days.
Improvement activities measures come in two categories, high-weight measures and medium-weight measures. High-weight measures are worth 20 points each. Medium-weight measures are worth 10 points each. To achieve maximum performance, you must report a combination of measures that equals 40 points.
If you choose two high-weight measures that would fulfill your 40-point requirement. If you choose all medium-weight measures you would need to report four measures. And obviously, the other option is one high-weight and two medium-weight measures.
Small Practices and the Improvement Activities Category
CMS has made accommodations for small practices. Anyone with less than 15 Eligible Clinicians or Rural Health and Health Professional Shortage Areas have their point worth doubled. A high-weight measure is worth 40 points and medium-weight measures are worth 20 points. Essentially, anybody in one of those qualifying categories would only need to do one high-weight activity or two medium weight activities to receive full credit for this category.
Selecting your Improvement Activities measures
When selecting your measures, there are a couple of things to keep in mind. In this article, I point out a few activities that I recommend you consider in your planning.
Bonus eligible Improvement Activities measures
This might be the only confusing part about the Improvement Activities category of MIPS. There are certain Improvement Activities that actually award you bonus points in the Advancing Care Information category. These measures are identified as Improvement Activities that CEHRT could be used for the activity. When choosing your IA measures, consider which of these measures will afford you a 10-point bonus in the Advancing Care Information category. The Quality Payment Program website has a PDF that lists all of the IA measures that are eligible for the ACI bonus points.
High-Weight Activities
Let’s take a look at some examples of high-weight activities. These activities range from population management to beneficiary engagement with a focus on how you care for Medicare and Medicaid patients. Many of these activities also look to integrate behavioral and mental health into practices.
I have highlighted two measures below that I believe you should pay attention to.
* Please note that this list of IA measures is only a sampling of the full list of Improvement Activities measures. For the full list of measures visit, https://qpp.cms.gov/measures/ia.
|
Activity Name |
Subcategory Name |
Weighting |
|---|---|---|
|
Anticoagulant management improvements |
Population Management |
High |
|
Collection and follow-up on patient experience and satisfaction data on beneficiary engagement |
Beneficiary Engagement |
High |
|
Consultation of the Prescription Drug Monitoring Program |
Patient Safety & Practice Assessment |
High |
|
Engagement of new Medicaid patients & follow-up |
Achieving Health Equity |
High |
|
Glycemic management services |
Population Management |
High |
|
Implementation of co-location PCP & MH services |
Behavioral and Mental Health |
High |
|
Implementation of integrated PCBH model |
Behavior and Mental Health |
High |
|
Participation in a 60-day+ effort to support domestic of international humanitarian needs |
Emergency Response & Preparedness |
High |
|
Participation in CAHPS or other supplemental questionnaire |
Patient Safety & Practice Assessment |
High |
|
Participation in systematic anti-coagulation program |
Population Management |
High |
|
Provide 24/7 access to eligible clinicians or groups who have real-time access to medical records |
Expanded Practice Access |
High |
The first measure I highlighted above is the Participation in CAHPS or other supplemental questionnaire. Many clinicians are already doing the CAHPS patient satisfaction survey. This may be an easy high-weight measure for you to complete if you already have engaged with a vendor that will administer that survey for you. Confirm with your vendor that they are using the CAHPS for MIPS survey for Medicare patients only.
Not only would this high-weighted activity give you 20 points in the IA category, but it would also give you credit for one high priority measure in the MIPS Quality category.
I’d also like to point out the measure, Provide 24/7 access to Eligible Clinicians or groups who have real-time access to patient’s medical record. This is also a high-weight measure and will most certainly improve your practice.
By taking a look at the guidance for this measure, you’ll see that there are options for how to demonstrate that you have fulfilled this measure.
* Guidance for all Improvement Activities measures are found again on the Quality Payment Program website.
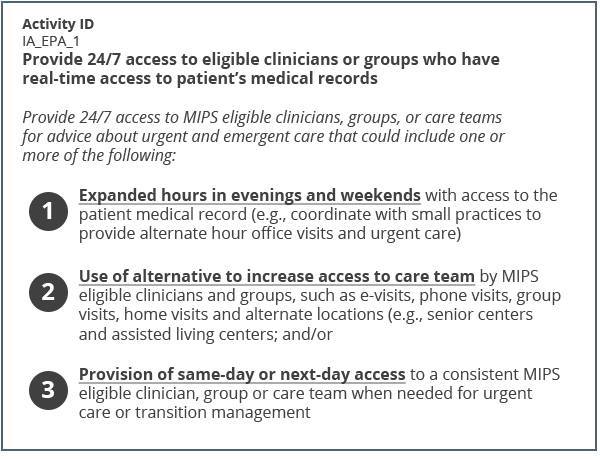
CMS has stated that they do not intend to offer any further guidance on these measures than what you see above. I suggest that you read the measure and decide how you are going to carry out the measure and document the activity.
CMS did say that you don’t have to do all of the activities listed. You may do just one or more of the activities they suggest. Perhaps you could expand your hours in the evenings and the weekends because you’re partnering with another clinic or practice. You might find other ways to increase your access, either by doing e-visits or phone visits, or maybe you could improve the way you provide same-day or next-day access. Each measure features different ways you can fulfill that measure's requirement.
Medium-Weight Activities
The medium-weight activities have similar variability of focus. I suggest that you examine these measures closely. For instance, if you just glanced through the activity names below, you might think to yourself, “Oh, diabetes screening, that’s easy.” But if you read this measure carefully, you’ll realize it’s diabetes screening for people with schizophrenia. Take this as a caution to investigate each measure fully before committing to improving that measure.
|
Activity Name |
Subcategory Name |
Weighting |
|---|---|---|
|
Care transition documentation practice improvements |
Care Coordination |
Medium |
|
Collection and use of patient experience and satisfaction data on access |
Expanded Practice Access |
Medium |
|
Diabetes screening |
Behavioral and Mental Health |
Medium |
|
Implementation of documentation improvements for practice/process improvements |
Care Coordination |
Medium |
|
Implementation of fall screening and assessment programs |
Patient Safety & Practice Assessment |
Medium |
|
Implementation of formal quality improvement methods, practice changes or other practice improvement processes |
Patient Safety & Practice Assessment |
Medium |
|
Implementation of improvements that contribute to more timely communication of test results |
Care Coordination |
Medium |
|
Improved practices that engage patients pre-visit |
Beneficiary Engagement |
Medium |
|
Measurement and improvement at the practice and panel level |
Patient Safety & Practice Assessment |
Medium |
|
Use group visits fro common chronic conditions |
Beneficiary Engagement |
Medium |
|
Use of decision support and standardized treatment protocols |
Patient Safety & Practice Assessment |
Medium |
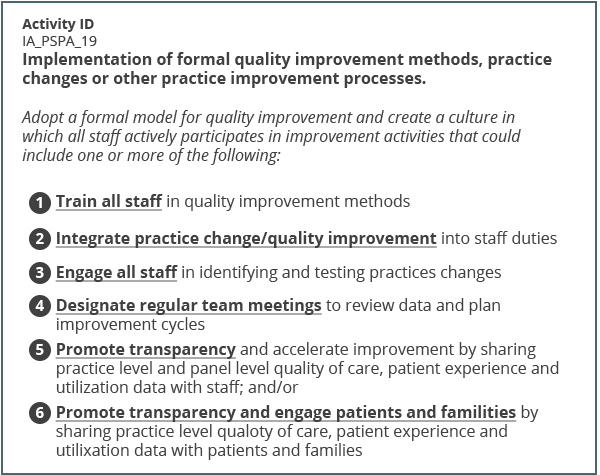
The measure that I have highlighted above is, Implementation of a formal quality improvement methods, practice changes or other practice improvement processes. In my opinion, this is a good one to focus on. If your practice has not done a lot of formal quality improvement in the ambulatory space, this can get you going. I would focus on some of the quality measures that you need improvement on and build it right around that. This measure would be worth 10 points and the activities are listed below.
Reporting Improvement Activities measures
Here are some additional cautions for this category.
Report one measure once
Each of the 92 Improvement Activities measures have an Activity ID. When we as a vendor report which measures you are submitting to MIPS, we are going to use that Activity ID. Even though you might be able to design multiple improvement projects around this one Improvement Activity, CMS only permits you to submit that Activity ID once. That’s not to say you can’t have multiple improvement activities going on for this measure, you just can’t get all of your category points by using one measure.
Report for 90 days
You must report your work on these measures for a minimum of 90 consecutive days. However, they don’t need to be the same 90 consecutive days for each measure. You can work on different measures at different times of the year.
Retain evidence of improvement
Keep evidence as you work on improving those measures for 90 consecutive days. Take a measurement at the beginning and at the end of your 90 days and compare your results, so you have proof that you did or did not make any improvement.
Patient Center Medical Homes
If you are a recognized Patient Center Medical Home (PCMH), you get all of the points for this category without submitting any measures. You’ll get credit for the full 15% category weight. Certain Alternative Payment Model participants also get full credit this year. Some get half credit. It’s your job to figure out if you are a recognized PCMH or an eligible APM participant.
Bear in mind that you must have been recognized as a PCMH by January 1 of 2017 to get full credit. If you are unsure of your status, the Quality Payment Program website has a phone number and email system at the bottom of their website, where you can ask the MIPS staff your question.
Tips for the Improvement Activities Category
In summary, here are my top tips to succeed in the Improvement Activities category of MIPS.
- Aim for 40 points which will give you the full category credit of 15% of your total MIPS composite score.
- Select at least one IA measure that is designated for ACI bonus points.
- Choose measures that you are already working on but haven’t formalized the process for. Or choose measures that are pertinent to your group.
- Document your starting point.
- Keep evidence of your work on the measure.
- Measures do not need to be from the same 90-day consecutive time frame.
- Confirm that you were recognized by January 1, 2017 as a PCMH or qualifying APM.
To get started in this category, it’s best to determine your 2017 reporting plans. Which measures are you going to report and what time of the year? Decide if you will be reporting as an individual or a group. Determine which reporting method you will use, attestation, EHR, etc. Find a reporting vendor (like Medisolv) that will help you submit all of your MIPS category requirements from one software system. Then have your organization agree to the plan, document and retain proof for at least six years in case of CMS audits.
FREE WEBINAR:
SURVIVING MIPS IN YEAR 2
Preparing For MIPS Reporting In 2018
This free educational webinar will help you understand who is eligible for the MIPS program and what’s required for successful completion. We will outline strategies that will help you prepare your providers for their best reporting year yet.
In this webinar, you will learn:
- About the changes made in the 2018 final rule for the Quality Payment Program;
- Reporting requirements for MIPS;
- How the final score is calculated;
- Best practices and resources for preparing your clinicians for a successful quality reporting year.


.png?width=352&name=2026%20Quality%20Reporting%20Deadlines%20Guide%20(1).png)



Comments