Using Your eCQM Data for COVID-19 Process Improvement
Read our COVID Mortality Analysis of 547 Medisolv Hospitals Over Nine Months.
We are on an ever-evolving COVID-19 treatment path. A year ago, your hospital was worried about diagnosing COVID-19 patients, keeping them alive and finding effective treatments. Not to mention the entire litany of other problems like evaporating supply chains, incorporating telehealth and reporting endless COVID-19 patient counts to the government.
As time progressed, more concrete treatment methods were established, and mortality rates leveled out. Hospitals began operating in this new normal where nothing is great but at least we had some literature to study.
Now, a year later. Where do we go from here? What do we focus on?
There have been several interesting studies about the long-term cardiovascular effects on a patient who had a severe COVID-19 case.
In fact, CMS and The Joint Commission have indicated that they are closely monitoring the VTE and Stroke performance measure results since COVID has entered the picture.
As a Quality leader, what does this mean to you and how can you help? The data you need is at your fingertips. Let’s figure out how to put it to work and create positive change for our recovered COVID-19 patients.
What the research says
In a recent JAMA study 78% of hospitalized patients who had recently recovered from COVID-19 had cardiac involvement and 60% experienced ongoing myocardial inflammation. These were patients who did not have any of these as preexisting conditions.
A separate study indicated that ongoing symptoms in recovering COVID-19 hospitalized patients is common. In their study ~80% of recovered COVID-19 patients had cardiac involvement while 25% showed evidence of ongoing myocardial inflammation.
It has now been well documented that COVID-19 patients could experience a lengthy recovery from their COVID-19 illness. But how long and what are the hospital readmission risks associated with their recovery time?
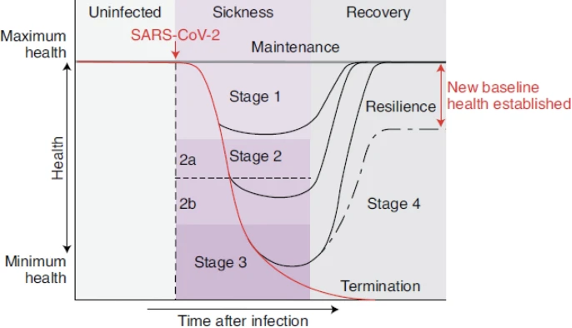
This study provided a pretty good graph documenting the separate recovery paths that COVID-19 patients take.
Source: Ayres, J.S. A metabolic handbook for the COVID-19 pandemic. Nat Metab 2, 572–585 (2020). https://doi.org/10.1038/s42255-020-0237-2
For some patients, there is never (at least not yet) a full recovery. There is only a new baseline health established.
So where might your hospital be seeing some of the subtle, long-term consequences of COVID-19? One place to begin your search is in your eCQM performance results.
Where do you find the data?
One of the first things I did after reading through some of these reports is analyze what I’m seeing in my clients’ data. I talked through the reports with a couple of clients and together we examined how their VTE and Stroke eCQM performance rates were trending.
One important thing to note here is that there are other long-term effects patients may experience such as respiratory effects. For this article, I focused on the cardiovascular effects since as Quality leaders we have visibility into these effects using readily available eCQM data.
Let’s start with VTE. I identified a few clients that typically do well with the VTE measure. We reviewed the patients who fell out of the measure. That’s the terminology we use to talk about patients who didn’t successfully complete the measure. When I cross examined those fallouts with the list of conditions, I noticed that several of these patients also had COVID-19.
Of course, this is just an anecdotal analysis. But given the research we do have that indicates the COVID-19 virus can attack the circulatory system, it raises some interesting Quality questions.
How many of those fallouts have returned to the hospital with a VTE or pulmonary embolism? How could the process be improved so that doesn’t happen? Should a greater emphasis be placed on pharmacological prophylaxis for a period of time after COVID-19 as a precaution? What is the “process improvement” for better quality of care for patients?
Keep in mind, COVID didn’t cause the fallouts, but the fallouts indicate that there needs to be a greater emphasis placed on prophylaxis due to the effect of the virus on the cardiovascular system. Looking at fallouts and those specifically with a COVID-19 diagnosis can be part of a process improvement initiative to be more cognizant of the importance of prophylaxis for these patients.
Moving on to stroke. Research shows that there is an increased rate of stroke on patients under the age of 50 who had COVID-19. As a result of the research, it may be beneficial for you take a look at your stroke eCQM Initial Patient Population and compare it to previous years. Are you seeing any change in the numbers? If you are seeing an uptick, can you identify which age group is seeing the increase? Take it a step further by creating a COVID-19 patient cohort. Do you see any correlation? Get together with your Quality team and come up with some ideas for process improvement. Are there any steps your hospital can take to prevent a post- or current COVID-19 patient from having a stroke?
We all know it’s as much about taking care of the current patient as it is about preventing the future patient from entering our hospitals. Starting this year, CMS is asking hospitals to voluntarily report the new Hybrid Hospital-Wide Readmission Measure. This brand-new type of measure combines your claims and EHR data to create a risk-adjusted readmission measure that will be used as part of your hospital IQR program.
Even though there is still very little known about COVID-19 and the long-term effects on a patient, we may be able to identify trends within our own environments and then take action to interpret and improve those processes. And it will likely have long term consequences, like having an impact on your hybrid readmission measure performance rate.
In fact, because COVID-19 patients ages 65 and older (i.e., Medicare patients) have the highest mortality rates, it wouldn’t surprise me if CMS adds a COVID-19 lab to the list of CCDEs for calculating future hybrid measure readmission rates.
I know. All this analysis and process improvement seems like a lot to ask when we are still struggling with the day-to-day tasks of managing a Quality department amid a pandemic. But the work we put in now to care for our recovered COVID-19 patients may have long-term consequences we can only distantly imagine.
Source List:1. https://www.jointcommission.org/resources/news-and-multimedia/news/2020/12/joint-commission-questionnaire-identifies-covid-19-impact/
2. Puntmann VO, Carerj ML, Wieters I, et al. Outcomes of Cardiovascular Magnetic Resonance Imaging in Patients Recently Recovered From Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020;5(11):1265–1273. doi:10.1001/jamacardio.2020.3557
3. Becker, R.C. Anticipating the long-term cardiovascular effects of COVID-19. J Thromb Thrombolysis 50, 512–524 (2020). https://doi.org/10.1007/s11239-020-02266-6
4. Ayres, J.S. A metabolic handbook for the COVID-19 pandemic. Nat Metab 2, 572–585 (2020). https://doi.org/10.1038/s42255-020-0237-2
5. https://www.nature.com/articles/s42255-020-0237-2
|
Medisolv Can Help
Here are some resources that might be helpful: |



.png?width=352&name=BlogImage_State%20of%20IQROQR%20Survey%20(4).png)

Comments