Value-Based Care vs. Fee for Service: Are We There Yet?

The healthcare industry’s journey from fee-for-service reimbursement to value-based reimbursement has been long and slow. How far have we come? And how far do we still need to go?
Value-Based Care vs. Fee for Service: Are We There Yet?
"Are we there yet?"
It’s a phrase most of us know well. We said it from the backseat to our parents on what we felt was an excruciatingly long car ride.
What do parents do when they hear that dreaded utterance from the backseat? Throw a few more snacks into the backseat to buy some time? Step on the gas? Or take a new route that will get them there faster?
The journey from fee-for-service reimbursement to value-based reimbursement has been a lot like that for the healthcare industry. It’s been an excruciatingly long ride. Advocates of the transition to value-based care, including quality leaders like you working at hospitals and health systems, are asking, “Why aren’t we there yet?” and “What do we have to do to get there?” Before we try to answer those questions, let’s look at where we started and where we are now.
Value-based care definition and origin story
The value-based care model has its roots in the mid-1970s, when the federal and state governments enabled the creation of health maintenance organizations. HMOs paid providers a capitated rate—a set payment per member per month—for the care they delivered to members. It was up to providers to figure out how to do that in a cost-effective manner without jeopardizing the health and safety of patients under their care.
But the official start of the race to value-based care, sometimes known as fee-for-value, is more recent—2015, to be exact. In January of that year, the U.S. Department of Health and Human Services (HHS) announced that it had set a goal.
By 2018:
- 90% of Medicare fee-for-service payments are tied to quality or value and
- 50% of Medicare fee-for-service payments are tied to alternative payment models (APMs)
HHS said it wanted most (90%) of what Medicare pays providers to flow through programs that quality leaders like you are very familiar with, like:
- The Merit-Based Incentive Payment System (MIPS)
- Hospital Readmissions Reduction Program (HRRP)
- Hospital Value-Based Purchasing Program (HVBPP)
- Hospital-Acquired Condition Reduction Program (HACRP)
- Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS)
HHS formed something called the Health Care Payment Learning and Action Network, or HCPLAN. Think of HCPLAN as the official scorekeeper of the shift to value-based care.
So, have we achieved value-based reimbursement yet?
According to industry experts, the answer is a resounding “No.”
At a panel discussion on the shift to value-based care at the recent ViVE conference in Miami Beach, Fla., the four members of the guest panel subjectively, unanimously and emphatically said we’re just not there yet.
From an objective standpoint, the four experts were right, according to the latest annual scorecard from HCPLAN. But we are getting closer.
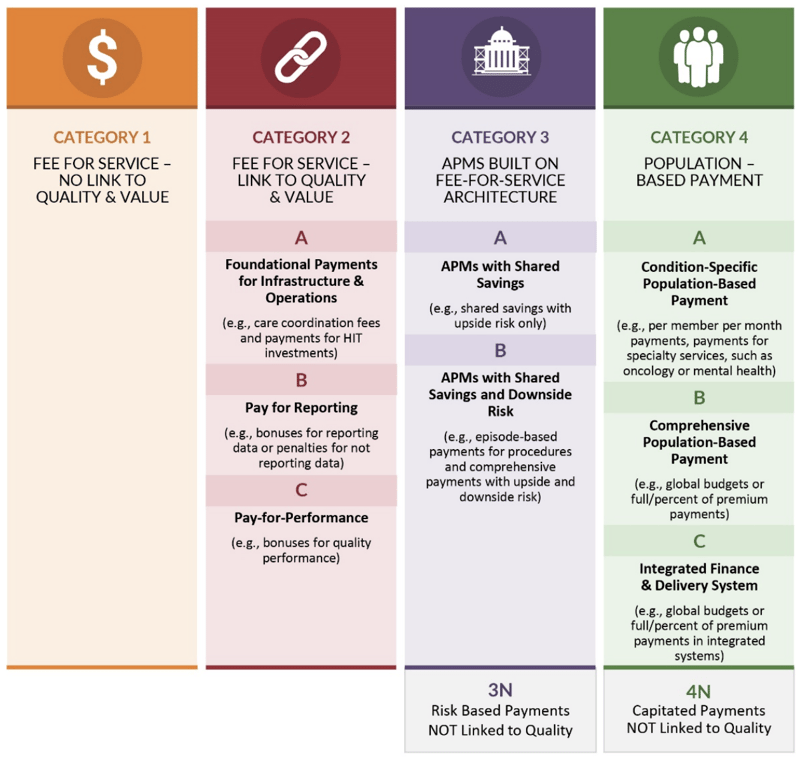
The HCPLAN breaks down payments to providers into four categories:
Category 1: Fee-for-service with no link to quality or value
Category 2: Fee-for-service tied to quality and/or value (this category is where most of your regulatory reporting falls; for example, IQR and MIPS)
Category 3: APMs built on a fee-for-service architecture
Category 4: Population-based payment
In 2020, 85% of traditional Medicare fee-for-service payments flowed through categories 2, 3 and 4, while 42.8% flowed through categories 3 and 4 only (APMs).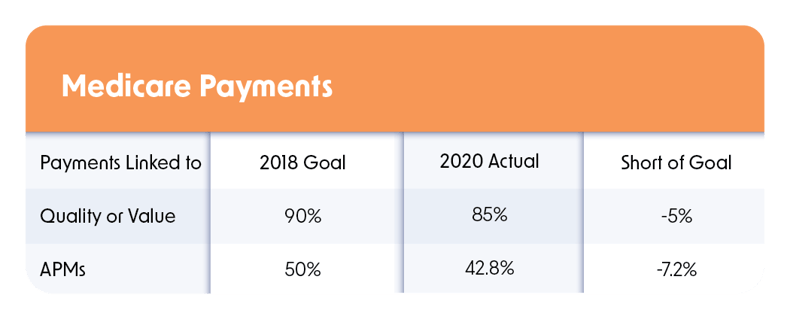
When you factor in payments from commercial health plans, Medicaid and Medicare Advantage plans, those numbers change in a very interesting way: They drop.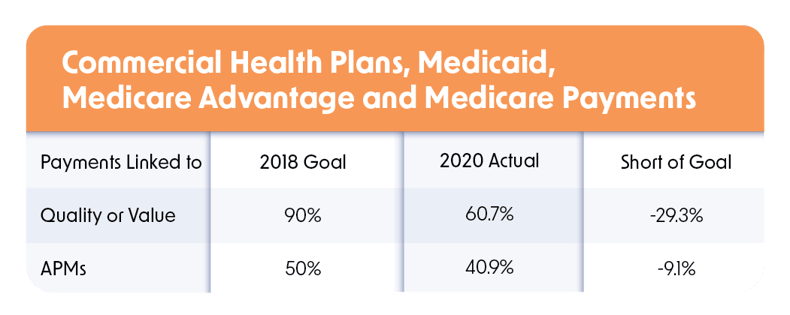
This means traditional Medicare, though behind HHS’s goals, is still leading other payers in making the shift to fee-for-value.
Reaching our value-based care destination
Subjectively and objectively, we’re not there yet, although we’ve made slow-but-sure progress. Yet, as we all know, the last mile (if you’re a runner) is always the toughest. What do we have to do to cross the finish line? The HCPLAN report identified some of the hurdles the industry needs to jump to make the transition to fee-for-value. The top three hurdles, according to payers surveyed for the report, are:
- Providers’ willingness to take on financial risk
- Providers’ ability to operationalize value-based care models
- Providers’ interest and/or readiness to transition to value-based care
What can quality leaders do to help their hospitals or health systems progress? Likely there’s not much you can do about the first hurdle. In fact, many experts believe that the amount of upside or downside financial risk isn’t big enough to make providers embrace value-based care payment models. (Think of how financially disappointing the MIPS reimbursement model is.) And that won’t happen until providers’ and payers’ financial incentives are aligned.
But there is something quality leaders can do about the second and third hurdles. For example, evaluate your system as a whole (the parts you have visibility into). Are there any areas of payment that fall into the first category of fee-for-service – no link to quality or value? Work on this low hanging fruit to start.
Most likely, you are responsible for much of what falls into the second category – again think of the reporting you do for MIPS and the reimbursements (or penalties) you get for the HAC, Readmission and Value-Based Payment programs.
What kind of progress could you make in this category? Are you getting a financial penalty in any of those programs? Could you eliminate that? How do you increase the incentive money you get in the MIPS or VBP programs? Consider tying provider performance in these categories to a financial incentive.
Beyond financial incentives, we’ve found that education is one of the keys to success. Don’t underestimate the power of information. When providers know 1) why it’s important to patient care, 2) the progress you’ve made collectively and 3) the goal and why it matters, things can change.
Your organization may or may not be already in category three. If you are associated with an MSSP ACO (Medicare Shared Savings Program Accountable Care Organization), then at least some of your providers are accounted for in this category.
Here’s where it becomes murky for you as a quality leader. How much visibility do you have into your physicians who fall in this category? Does your ACO provide feedback on how your providers’ performance compares to others in their ACO? What can you do expand this model to other aspects of your business?
Category 4 feels like a pipe dream for most organizations at this point. Less than 7% of payments are made to providers in this category.
Our suggestion is to focus on eliminating category one payments, improving your performance in category 2 (seeing if you can align financial and quality initiatives) and consider expanding category 3 participation.
Having a firm and demonstrable grasp on the connection between quality and financial performance will make entering into value-based care arrangements with payers something to pursue rather than flee from.
So, while we’re not there yet, we’re well on our way.
Learn more about Medisolv’s ENCOR for Electronic Clinician Measures and Value Maximizer software programs that can help your hospital or health system successfully navigate CMS’ value-based performance programs.
Medisolv Can HelpAlong with award-winning software, each client receives a dedicated Clinical Quality Advisor that helps you with your technical and clinical needs. We consistently hear from our clients that the biggest differentiator between Medisolv and other vendors is the level of one-of-one support. Especially if you use an EHR vendor right now, you’ll notice a huge difference.
|



.png?width=352&name=BlogImage_State%20of%20IQROQR%20Survey%20(4).png)

Comments