What is Data Completeness in MIPS?

CMS is sunsetting the CMS Web Interface reporting option for MSSP ACOs effective January 1, 2025. For an ACO staring at dozens of practices across multiple EMRs it can lead them to ask, "do I really need to gather data across all practices? What about practices who can't generate QRDA I files? What about my paper practices?"
As ACOs grapple with the scope of the work, one of the most common questions I get has to do with a term CMS calls Data Completeness. What is it and how many practices do I need to include in my submission to CMS?
CMS released a new guide to Data Completeness that further validates the 100% of eligible patients. They make it very clear that no one can be excluded from the Denominator population.
Data Completeness Requirements
There has been SO MUCH discussion on this topic. I once watched an ACO representative grill a CMS representative in a live panel discussion for no less than 20 mins on this topic. I think we all left even more confused. CMS attempted to make it clearer (which they are terrible at). So, here’s the best summary and documentation I can offer you.
An ACO must submit their entire “universe” of patients. None of your practices can be excluded based on populations. The data completeness threshold really would only be applicable in a MIPS CQM situation and even in that situation you still must have the entire universe of practices/patients and only achieve 70% completeness on the denominator patients.
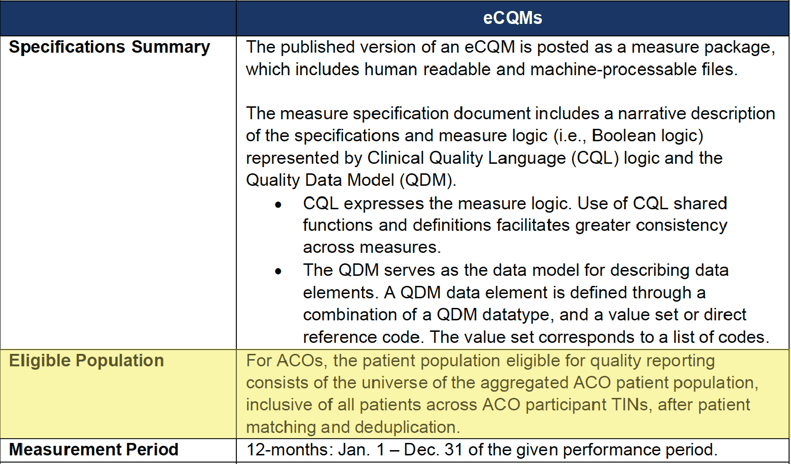
Take a look at pages six and eight of the APP guidance document here.
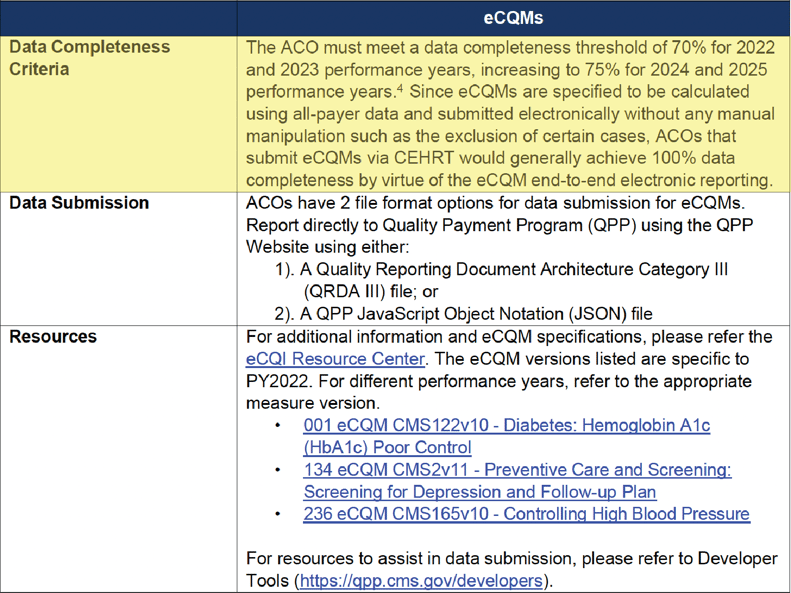
eCQM Data Completeness Criteria Summary
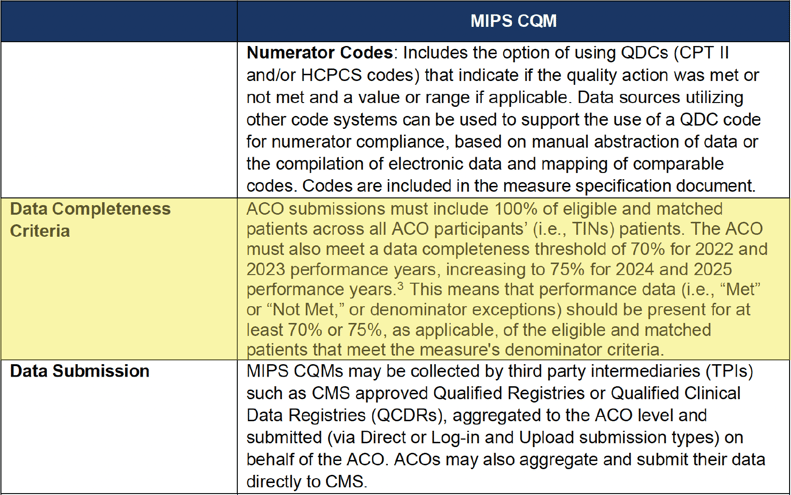
MIPS CQM Data Completeness Criteria Summary
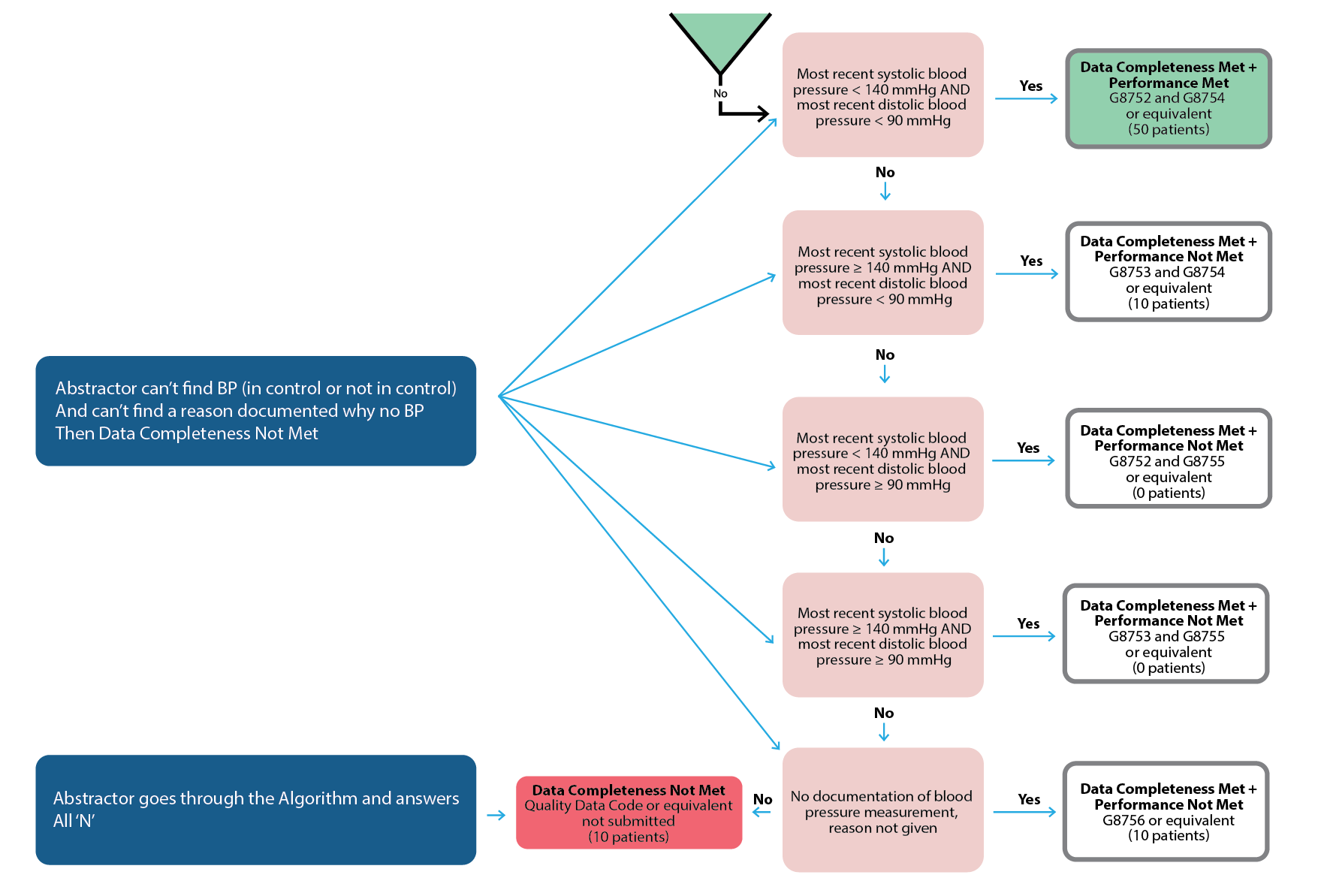
When is the data completeness threshold applicable?
It’s an unlikely scenario. But in some cases, an abstractor can't find the documentation that’s required by the measure. In this red scenario below an abstractor answers “no” to algorithm questions for more than 30% of cases.
How to Get Started With eCQM/CQM Reporting
ACOs must learn to juggle multiple, disparate EHRs and data collection methodologies. Developing a cohesive data aggregation system is going to be a major undertaking. Your senior leadership, quality management, and information technology teams need to start planning what that looks like for your ACO now.
The most important thing you can do right now is understand what your data landscape looks like. Here are a couple of questions you should know.
- Which practices are on which EMRs? Make a list.
- How many instances of each EMR vendor do you have?
- Do you have any practices still on paper charts? (<<If so, you cannot report to CMS.)
- How many practices are on less common EMRs?
- Can every single practice generate a QRDA I file (<<Applicable for eCQMs. Especially focus on those practices with less common EMRs.)
- Do you capture CPT II (G codes) in a database for all practices? (<<Applicable for MIPS CQMs/Medicare CQMs.)
This information will help you to choose whether you want to submit eCQMs, MIPS CQMs or Medicare CQMs. It will also inform you as to whether or not you have to set up conversations with any practices not able to provide your group with what you need.
How Long Will the Data Acquisition Process Take?
This is completely dependent upon your organization set up. For most of our clients, we tell them to estimate a 6–8-month implementation time before you start to see any meaningful data.
Final Thoughts: Don’t Wait
Yes, it’s true. History has proven that CMS could change the rules and deadlines on us any minute, however, in the 2023 final rule CMS made it clear that they are still intending to sunset the CMS Web Interface Measures by 2025 for everyone.
It's in your best interest to start looking at your data through the all-patients, all-payers, all-practices lens now. It is the key to unlocking so many other patient care goals for you, including improving population health, reducing health care costs, and advancing health equity. For too long, the CMS Web Interface had made quality reporting a box that organizations had to check. It’s time now for organizations like yours to lead the charge to elevate the role of quality data in patient care. Together, we have the power to put quality data to good use.
More Resources to Prepare Your ACO For What’s Next
At Medisolv, we offer so much more than quality software and start-to-finish submissions management. We’re the quality improvement partner committed to deciphering and anticipating CMS’s regulatory changes for you—so that you can keep your organization ahead of the curve.
Check out some of our additional resources now:
- eBook: CMS Web Interface Transition Guide
- Article: 2023 QPP Requirements
- On-Demand Webinar: Preparing your ACO for APP Reporting
Medisolv Can HelpAlong with award-winning software, each client receives a dedicated Clinical Quality Advisor that helps you with your technical and clinical needs. We consistently hear from our clients that the biggest differentiator between Medisolv and other vendors is the level of one-of-one support. Especially if you use an EHR vendor right now, you’ll notice a huge difference.
|

.png?width=352&name=2026%20Quality%20Reporting%20Deadlines%20Guide%20(1).png)



Comments