A Beginner's Guide to MIPS Year Two: 2018

The new year is creeping up on us, which can only mean one thing. No, I'm not talking about a fresh start with new resolutions or even the holiday spirit. It means CMS dropped the final rule for the Quality Payment Program. Did you just get chills? Me too, and I can assure you that it's not from the colder weather. You're now panicking that this MIPS program is quickly heading into year two and you're still sorting out how you'll manage year one.
Well, grab a cozy blanket because we've got a good read. In this blog we cover the MIPS Year Two requirements.
If you would like to use this blog as an ongoing resource, be sure to download and print our free 31-page eBook at the bottom of the page.
WHAT IS MIPS?
The history of MIPS
In 2015, Congress passed a bill for Medicare payment reform that is designed to lower health care costs and improve the quality of patient care.
From the Medicare Access and CHIP Reauthorization Act (MACRA) legislation was born the Quality Payment Program.
The Quality Payment Program
The Quality Payment Program combines previous provider reporting programs (PQRS, Meaningful Use and Value-Based Modifier) into one comprehensive program.
Those eligible to report to the Quality Payment Program will report under one of two tracks.
Track 1: MIPS
Merit-Based Incentive Payment System
Those eligible for the MIPS track are required to report clinician performance across four categories related to quality and patient safety performance.
Track 2: AAPM
Advanced Alternative Payment System
Advanced APMs are a subset of APMs and let practices earn more for taking on some risk related to patients’ outcomes.
Who is Eligible for MIPS?
The following titles are eligible to be a part of the MIPS program.
- Physician
- Physician Assistant
- Nurse Practitioner
- Clinical Nurse Specialist
- Certified Registered Nurse Anesthetist
It’s not just a title that makes you eligible for this program. You must also bill Medicare more than $90,000 annually OR provide care for more than 200 Medicare patients a year.
Resource
You can easily check to see if you are eligible to participate in this program by visiting the Quality Payment Program website. Right on their homepage, they have an eligibility look up. You’ll need your NPI number.
PAYMENTS
What's at risk, what is there to gain?
If you are eligible and do not achieve the score threshold of the MIPS program, you’ll lose -5% of your Medicare fee reimbursement to your 2020 payments. On the flip side, you can earn up to +5% PLUS bonus money for top performers.
Note: This payment adjustment will be made to your fiscal year 2020 Medicare fee schedule.
Category Requirements
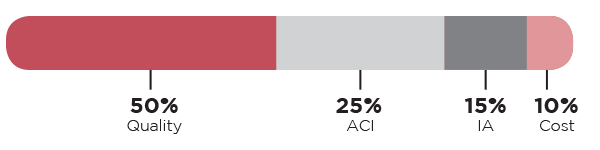
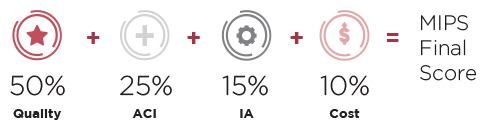
Each category of MIPS has a different set of requirements that you must follow in order to fully participate and have your best chance at making incentive money. In 2018, the Cost category has been added to count for 10% of your total MIPS score. The Quality category is now worth just 50% of your total score.
There are four categories that make up the MIPS program.
 |
 |
||
| Quality (Old PQRS program) |
Advancing Care Information (Old Meaningful Use program) |
Improvement Activities (New program) |
Cost (Old Value-Based Modifier program) |
Each of these categories carries a different weight. Your score in each category will be totaled into one composite MIPS score.
 QUALITY CATEGORY
QUALITY CATEGORY
Maximum Points: 60 points
Category is Worth: 50% of total MIPS score
Formerly: The PQRS Program
Performance Period: 365 days
Requirements:
| Report a total of six Quality measures to CMS. | |
| Submit at least one Outcome measure unless there is not one available in your specialty measure set. If that is the case, you can report another High Priority measure in its place. | |
| Submit 365 days' worth of 2018 data. | |
| If you are reporting via the CMS web interface, report 15 Quality measures. |
Other Considerations
CAHPS for MIPS
Submitting the MIPS CAHPS Survey, will count as reporting one High Priority measure. Select five other Quality measures to report, including an Outcome measure if available.
Case Minimum
Quality measures must meet the 20-case minimum to be scored.
Data Completeness
Measures must contain at least 60% of all Eligible Clinician patients across all payers.
 ADVANCING CARE INFORMATION CATEGORY
ADVANCING CARE INFORMATION CATEGORY
Maximum Points: 155 possible points, but capped at 100 points
Category is Worth: 25% of total MIPS score
Formerly: The EHR Incentive (Meaningful Use) Program
Performance Period: 90 days (minimum)
Requirements:
| Report all four Base measures. | |
| Choose from seven Performance measures and submit enough to reach the 100-point threshold. |
Other Considerations
Base Submission Requirement
You MUST report ALL BASE measures. If you do not report ALL BASE measures you will receive zero points in the ACI category, regardless of how well you do with the ACI Performance measures.
Note: If you have achieved Meaningful Use Stage 3 Functionality and have the 2015 EHR Certification you may choose to submit the advanced Base measure set instead.
Reassigning ACI points to Quality
If you feel that the ACI measures aren’t relevant, you can request from CMS that they reassign the ACI percent of your score to the Quality category. If approved, you would have 75% of your MIPS total score attributed to your Quality score and the remaining 25% would be from your Improvement Activities and Cost scores.
 IMPROVEMENT ACTIVITIES CATEGORY
IMPROVEMENT ACTIVITIES CATEGORY
Maximum Points: 40 points
Category is Worth: 15% of total MIPS score
Formerly: New Category
Performance Period: 90 days (minimum)
Requirements:
| Report a combination of Improvement Activity measures (up to four measures) to equal a total of 40 points. | |
| Groups with <15 participants in a rural or health professional shortage area may attest to two Improvement Activities for 90 days (minimum). |
Note: If you are Patient-Centered Medical Home and more than 50% of your practices are recognized as a PCMH, you automatically receive full credit for this category.
 COST
COST
Category is Worth: 10% of total MIPS score
Formerly: Value-Based Modifier
Performance Period: 365 days
Requirements:
The Cost category is new for 2018. This category will only include the Medicare Spending per Beneficiary (MSPB) and total per capita cost measures in 2018 to calculate cost score.
Clinicians will receive a score for their performance on these two Claims measures. No additional data submission is required to calculate the claims measure rates.
Reporting Options
In 2018, you may choose to report as an individual hospital, group, large practice or virtual group.
Individual
This is defined as a single National Provider Identifier (NPI) tied to a single Tax Identification Number (TIN). Your hospital will report individual data for each MIPS category.
Group
Reporting as a group is defined as a set of clinicians (identified by their NPIs) sharing a common TIN. You must report group-level data for each MIPS category.
Large Practice
Optionally, large practices with >25 providers may choose to report via the CMS Web Interface. In this reporting option you must report 30+ measures with a full year’s worth of data.
Note: If you plan to submit using the CMS web interface you must tell CMS by June 30, 2018.
Virtual Group
A virtual group will allow individual clinicians and small groups to come together to form one virtual group which can report together. Groups must be comprised of 10 or fewer Eligible Clinicians and, as a group, exceed the low-volume threshold.
Note: If you choose to participate in a Virtual Group, you must tell CMS prior to December 31, 2017.
Technical Requirements
EHR Requirements
CMS did a good job of scaring everyone into thinking they had to be ready to use the 2015 Edition of Certified EHR Technology (CEHRT) in 2018. However, they are now permitting Eligible Clinicians to still use the 2014 Edition instead. While it’s no longer a requirement, CMS is encouraging the use of 2015 CEHRT with a 10% bonus for those who exclusively use the 2015 Edition.
MIPS SCORING
MIPS Final Score
How to make money in MIPS
To avoid at -5% penalty, you must score at least 15 points.
To be eligible for bonus money you must score at least 70 points (Exceptional Performance Bonus).
Reimbursements
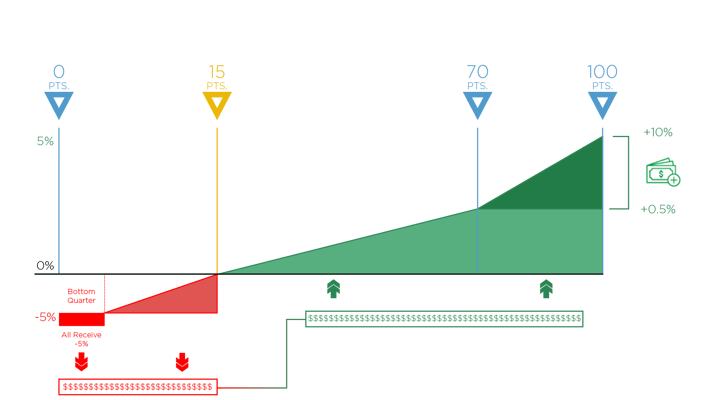
0-14 Points
If you do not meet the 15-point, performance threshold in 2018, you will automatically have -5% reduced from your 2020 Medicare fee schedule (in red above).
15-100 Points
CMS will take the funds of those who did not meet the threshold (in red) and distribute them among those who did meet the threshold (in green). Anyone whose MIPS score is between 15 and 100 points will receive some portion of those funds – up to a 5% increase to their 2020 Medicare fee schedule.
70 Points
By scoring at least 70 points, you’ll be eligible for the Exceptional Performance bonus money (on the right). CMS has set aside an additional $500 million to distribute to anyone who scores between 70 – 100 points. This is on top of whatever portion of money you receive from those who do not participate (in red).
Bonus Points
There are many opportunities to get bonus points within the MIPS program.
Improvement Bonus: Up to 10 Points
Clinicians will be rewarded if they demonstrate any improvement to their 2018 Quality and or Cost score over last year (pending there is enough data for comparison).
CEHRT Submission: Up to 6 Points
Receive up to 6 bonus points by submitting your Quality measures via CEHRT submission.
Additional Measure Submission: Up to 6 Points
By submitting additional Outcome, Patient Experience or High Priority measures in the Quality category, you can be rewarded up to 6 bonus points.
ACI Bonus Points: Up to 10 Points
By choosing to report select Improvement Activities measures you can receive bonus points in the Advancing Care Information category.
Public Health Registry Measure Bonus: Up to 10 Points
Up to 10 points are available for those who report an additional registry measure in the ACI category,
2015 Edition of CEHRT Bonus: Up to 10%
Report 90 days of ACI measures using the 2015 edition of CEHRT to get the 10% bonus on the ACI score.
Complex Cases Bonus: 1-3 Points
For clinicians who work with patients that have more complex cases, CMS will award up to 3 bonus points to the clinician’s MIPS final score.
Small Practice Bonus: 5 Points
An additional 5 bonus points will be added to the final MIPS score for anything qualifying as a small practice.
IMPORTANT DATES TO REMEMBER
It’s getting close to the beginning of the year now. If you haven’t prepared to start tracking your measures you have a slim margin to get ready. The date you need to remember is January 1, 2018. This is the start date to track 365 days of Quality and Cost category measures. For the Advancing Care Information category and the Improvement Activities category, you may start between January 1 and October 2, 2018 to track your measures at a 90-day minimum.
The last day to submit all of your performance data is April 2, 2019.
Resource: This Beginner's Guide to MIPS Year 2 eBook will give you a rundown of the basics of the MIPS program. It’s a handy reminder of what you are required to do and by what date.
Resource: Confused by the immense about of acronyms you read above? Download our Healthcare Quality Acronym Reference Guide to use as a quick cheat sheet.
Medisolv MIPS Package
Medisolv Can Help
Medisolv’s quality reporting software, ENCOR, is designed to meet your MIPS reporting needs. Our solution spans both the ambulatory and inpatient settings and includes consulting and submission services.
Learn how we can help you successfully submit to the Quality Payment Program. Contact one of our MIPS professionals >>
DOWNLOAD:
[e-book] A Beginner's Guide to MIPS Year 2
With the MIPS final rule in place, providers nationwide are trying to understand the changes for the year to come. MIPS offers unprecedented opportunities to substantially increase payments for exceptional performance.
Medisolv has the tools you need now to prepare.This FREE 31-page eBook is a beginner’s guide to the MIPS program Year 2. You'll learn about the basics of the Quality Payment Program under MIPS in 2018.
This guide includes:
- Eligibility criteria
- Reporting options
- Category requirements
- Important dates to remember
- An acronym definition section

.png?width=352&name=2026%20Quality%20Reporting%20Deadlines%20Guide%20(1).png)



Comments