MIPS Year Three: 14 Things to Know

It’s officially November, which means you definitely have the right to get a head start on holiday decorating. And in the health care world…it means that CMS has finalized their proposed changes to the Quality Payment Program (QPP) for 2019.
In the 2019 QPP final rule that was dropped late last week, CMS is working toward reducing clinician burden, giving patients access to their data, improving patient outcomes and supporting small and rural practices by making several adjustments to the MIPS program.
So, to help you start preparing for your MIPS duties in 2019, we’ve complied 14 MIPS highlights from the final rule below.
Note: CMS made a few changes to your 2019 MIPS requirements in response to COVID-19. Changes are noted below. Read our blog, to learn more about the overall changes to quality reporting in response to COVID-19.
1. Eligibility list expansion
Next year, a wider range of clinician types will be eligible to participate in MIPS.
In addition to the 2018 Eligible Clinician types (Physician, Physician assistant, Nurse practitioner, Clinical nurse specialist and Certified registered nurse anesthetist), the following clinicians have been added to the eligibility list for 2019:
- Physical therapist
- Occupational therapist
- Qualified speech-language pathologist
- Qualified audiologist
- Clinical psychologist
- Registered dietitian or nutrition professionals
2. Payment adjustment increase
In 2019, CMS is increasing the positive and negative payment adjustment by two percentage points. That’s right, folks—the stakes are higher, and the reward is greater.
That means that next year, you can earn a positive adjustment of up to +7% based on your performance in each MIPS category and a negative reduction of up to -7%. This is up from +5% and -5% in 2018.
3. Performance threshold increase
The performance threshold is increasing, too. To avoid a penalty in 2019, you’ll need to score at least 30 points compared to 15 points in 2018.
And to qualify for the Exceptional Performance Bonus money that CMS sets aside for exceptional performers, you’ll need to score 75 points now as opposed to 70.
Remember, since MIPS is a budget neutral program, CMS will take all the funds from the negative payment adjustment and distribute them among those who did meet the performance threshold and achieved the positive payment adjustment. So, any Eligible Clinician or group who scores 30-100 points will be able to get some portion of these funds.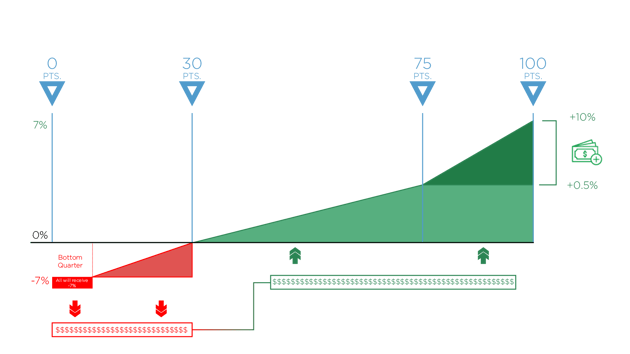
4. Another way to be excluded from MIPS
CMS is adding one more factor that can get you excluded from MIPS in 2019: You provide less than 200 covered professional services under the Physician Fee Schedule (PFS).So if you can say yes to any of these following factors, you will be excluded from MIPS in 2019.
You bill Medicare less than $90,000 annually.
OR
You provide care for less than 200 Medicare patients a year.
OR
You provide less than 200 covered professional services under the Physician Fee Schedule (PFS).
5. A new opt-in policy
That being said, even if you are excluded, you can still participate if you want to. CMS established a new opt-in policy for MIPS reporting next year. If an Eligible Clinician meets at least one of the three eligibility factors below, they can opt-in to the program in 2019.
You bill Medicare more than $90,000 annually.
OR
You provide care for more than 200 Medicare patients a year.
OR
You provide more than 200 covered professional services under the PFS.
6. Technology requirement change
Alas, the time has come. In 2019, you will be required to use the 2015 edition of CEHRT. Eligible Clinicians and groups will no longer have the option of using the 2014 edition. Womp womp.
*Raises hand.* Keep in mind that Medisolv is already certified to the 2015 edition of CEHRT. Need some help? Send us a note.
7. Advancing Care category renamed Promoting Interoperability
In case you missed it, the Advancing Care Information category has been renamed the Promoting Interoperability category. This name change reflects the changes that CMS is making to the category in an effort to support greater EHR Interoperability and patient access.
8. Category weight changes
Just as in 2018, there are four MIPS categories that will count toward your overall score in 2019: Quality, Improvement Activities (IA), Promoting Interoperability (PI, formerly Advancing Care Information) and Cost.
Unlike 2018 however, the percentage weight for the Quality category will decrease from 50% to 45%, while the percentage for the Cost category will increase from 10% to 15% next year. The weighting for the IA and PI categories will remain the same.
9. New MIPS Terms
CMS decided that some of the language they use was a little less than clear.
So they clarified a few things for us in 2019. Here are some name changes to watch out for.
- Collection Type: Essentially the names of the types of measures in each category.
- MIPS Clinical Quality Measures (CQMs) – formerly referred to as “Registry measures”
- Electronic Clinical Quality Measures (eCQMS)
- Qualified Clinical Data Registry (QCDR) measures
- Medicare Part B Claims measures
- CMS Web Interface measures
- The CAHPS for MIPS survey measure
- Administrative Claims measures
- Submitter Type: The person or group or vendor who is submitting the measures to CMS.
- Eligible Clinician
- Group
- Third party intermediary (i.e. Your pals at Medisolv)
- Submission Type: The way in which you submit your data to CMS.
- Direct
- Log in and upload
- Log in and attest
- Medicare Part B claims
- CMS Web Interface
10. Multiple submission options for the Quality category
The reporting requirements for the Quality category are not changing in 2019. You’ll still need to report a total of six Quality measures for a period of 365 days.
But next year, you can choose from multiple submission methods for a single measure rather than just one.
 Here are your options:
Here are your options:
- EHR (eCQMs)
- MIPS CQMs (Formerly called Registry)
- QCDR
- CMS web interface
- Claims
CMS will determine your score using the data submission with the greatest number of measure achievement points.
11. Eight new episode-based measures for the Cost category
In addition to the Medicare Spending per Beneficiary (MSPB) and the Total Per Capita Costs for All Attributed Beneficiaries (TPPC) measures that will be evaluated for your Cost score, CMS is adding eight new episode-based measures next year.
| Measure Name | Measure Type |
| Elective Outpatient Percutaneous Coronary Intervention (PCI) | Procedural |
| Knee Arthroplasty | Procedural |
| Revascularization for Lower Extremity Chronic Critical Limb Ischemia |
Procedural |
| Routine Cataract Removal with Intraocular Lens (IOL) Implantation | Procedural |
| Screening/Surveillance Colonoscopy | Procedural |
| Intracranial Hemorrhage or Cerebral Infarction | Acute inpatient medical condition |
| Simple Pneumonia with Hospitalization | Acute inpatient medical condition |
| ST-Elevation Myocardial Infarction (STEMI) with Percutaneous Coronary Intervention (PCI) |
Acute inpatient medical condition |
Your performance in all 10 of these measures will be compared with other MIPS Eligible Clinicians and groups in 2019.
*Note: In response to COVID-19, CMS will not calculate Cost as a part of your 2019 score. If, however, you submit your other data by the extended deadline, CMS will add the weight of your Cost score to your Quality score.
12. Scoring changes for the PI category
In the past, clinicians would have to submit all of the Base measures in this category before submitting additional Performance measures to successfully complete this category. This is changing for 2019. You’ll now be scored on your performance for each individual measure. CMS will add up each measure score to calculate your final score worth a maximum of 100 points.
And since you will now be required to use the 2015 edition of CEHRT, there will no longer be two measure path options. So, for 2019, you’ll report on a smaller set of objectives and measures.
| Objectives | Measures | Max Points |
| e-Prescribing |
e-Prescribing |
10 pts |
| Bonus: Query of Prescription Drug Monitoring Program (PDMP) | 5 bonus pts | |
| Bonus: Verify Opioid Treatment Agreement | 5 bonus pts | |
| Health Information Exchange |
Support Electronic Referral Loops by Sending Health Information |
20 pts |
| Support Electronic Referral Loops by Receiving and Incorporating Health Information | 20 pts | |
| Provider to Patient Exchange | Provide Patients Electronic Access to Their Health Information | 40 pts |
| Public Health and Clinical Data Exchange | Choose two: Immunization Registry Reporting, Electronic Case Reporting, Public Health Registry Reporting, Clinical Data Registry Reporting and Syndromic Surveillance Reporting | 10 pts |
13. IA adjustments
In 2019, CMS is making several adjustments to the IA category to align with its newest criterion—include a public health emergency as determined by the secretary and remove activities that may be considered for a PI bonus.Here’s what they plan to do next year:
- Add 6 new activities
- Modify 5 existing activities
- Remove 1 existing activity
- Discontinue the bonus points for IA measures that use CEHRT
14. Bonus Points
Here are a few bonus point modifications to note:
- The small practice bonus is increasing from 5 to 6 points, but it will only be available in the Quality category rather than being applied to the final MIPS score.
- Because the technology requirement is changing, the 10-point bonus that was previously available in the PI category for using the 2015 edition of CEHRT is no longer applicable. However, participants will still receive a bonus point for every measure they submit electronically in the Quality category.
Be sure to stay tuned for next week's post, where we break down all the MIPS requirements for 2019.
And keep in mind that when you partner with Medisolv, our clinical experts can walk you through the MIPS changes, year after year, to ensure a successful submission and the best possible MIPS score.
Medisolv MIPS PackageMedisolv Can HelpMedisolv’s quality reporting software, ENCOR, is designed to meet your MIPS reporting needs. Our solution spans both the ambulatory and inpatient settings and includes consulting and submission services. Learn how we can help you successfully submit to the Quality Payment Program. Contact one of our MIPS professionals >>
|

.png?width=352&name=2026%20Quality%20Reporting%20Deadlines%20Guide%20(1).png)



Comments