MIPS Year Two: 13 Things to Know [SLIDESHOW]
![MIPS Year Two: 13 Things to Know [SLIDESHOW]](https://blog.medisolv.com/hs-fs/hubfs/Blogs/11-2017/Featured-Image-13-Things.png?width=900&height=600&name=Featured-Image-13-Things.png)
As October closed, CMS announced a new initiative called the "Patients Over Paperwork" initiative. The goal is to reduce the regulatory reporting burden put on clinicians. CMS wants to continue their transition to paying for value and quality, but redefine what it means to pay for value and quality. Their new initiative “aims to focus on outcome-based measures going forward, as opposed to trying to micromanage processes.”
In the same week, CMS dropped the Quality Payment Program (QPP) final rule for year two. This new initiative is reflected in the changes found within the 1,653-page final rule. Based on the new requirements, it's clear that CMS is attempting to ease the transition into QPP for all clinicians and provide relief to small practices.
Also see: CMS QPP Year 2 Final Rule Executive Summary
We have pulled together the top 13 significant highlights from the final rule. Here’s what you can expect for MIPS in 2018.
(Use the arrows on the side of the slide to navigate between slides. Or download the PDF version.)
1. Eligibility Requirements
Eligibility requirements will change to make it easier for clinicians to be exempt from MIPS reporting. The same titles are eligible – Physician, Physician Assistant, Nurse Practitioner, Clinical Nurse Specialist, Certified Registered Nurse Anesthetist. In addition to these job titles the clinician must:
Bill Medicare more than $90,000 in allowable charges
OR
see more than 200 Medicare Part B patients.
Last year, clinicians were excluded if they billed Medicare less than $30,000 or saw less than 100 Medicare Part B patients. This change will exclude more clinicians from reporting in 2018.
2. EHR Technology
CMS did a good job of scaring everyone into thinking they had to be ready to use the 2015 Edition of Certified EHR Technology (CEHRT) in 2018. In the final rule, however, they have backed away from that requirement, now permitting Eligible Clinicians to still use the 2014 Edition instead. While it’s no longer a requirement, CMS is encouraging the use of 2015 CEHRT with a nice 10% bonus in the ACI category for those who exclusively use the 2015 Edition.
3. Category Weighting
In the proposed rule, CMS said they would keep the categories weighted the same as they were in 2017. However, in the final rule they changed their mind, stating that it would make the transition to 30% weight for Cost in 2019 more difficult. So in 2018, the Cost category will be weighted 10% of the final score, which means there is a change in the Quality category as well. The Quality category has bumped down from 60-50% of the total score. Here are the category weightings for 2018.

- Quality = 50% of total score
- Advancing Care Information = 25% of total score
- Improvement Activities = 15% of total score
- Cost = 10% of total score
4. Category Requirements
The only change comes within the Cost category. CMS will not use the 10 episode-based measures that are used for the 2017 MIPS performance period. The Cost category will only include the Medicare Spending per Beneficiary (MSPB) and total per capita cost measures in 2018.
All other categories - Quality, IA and ACI, do not have requirement changes. CMS has modified and added several measures in each category.
More details >> (Pages 8 - 16)
5. Reporting Options
No longer can you “Pick Your Pace” for reporting to MIPS. For the Quality and Cost categories you must submit 365 days of data. For the Improvement Activities (IA) and Advancing Care Information (ACI) categories you must submit a minimum of 90 days of data.

6. Quality data completeness
In 2017, all of the Quality measures that you submit must contain at least 50% of all Eligible Clinician patients across all payers. In 2018 this percentage is upped to 60%. If your measure fails this requirement you will earn only one point for that measure, instead of the possible 10 points.
If, however, you are considered a small practice, you will still earn a minimum of three points for each Quality measure submitted regardless of the percentage of patients included.
7. Performance Threshold
You must achieve at least 15 points to avoid a -5% penalty in 2018. That’s up from the three-point minimum of 2017. In the graph below, you’ll see the performance threshold minimum at 15 points and the performance threshold for exceptional performance at 70 points. Once you hit that 70-point threshold you will earn bonus money on top of any money you make from scoring above the 15-point threshold score.
More details >> (Pages 17 - 18)
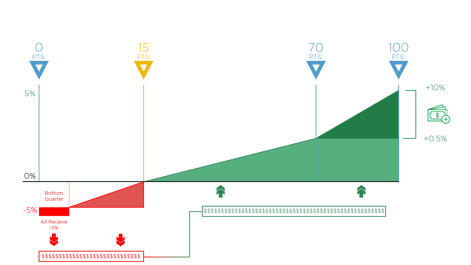
8. Payment Possibilities
And speaking of money, as I mentioned above, you can get up to 5% added to your Medicare reimbursement funds by performing well in MIPS next year. Conversely, you can expect to receive a -5% reduction to your Medicare reimbursement funds if you don’t meet that 15-point performance threshold score.

9. Help for Small Practices
Small practices get several breaks in this upcoming year, including the following:
- Five bonus points added to their MIPS final score;
- New hardship exceptions in the Advancing Care Information category;
- Continuing to award small practices three points for Quality measures that don’t meet the Data Completeness requirement;
- And increasing the low-volume threshold so that more small practices are exempt from MIPS.
More details >> (Pages 6, 8, 16 and 17)
10. Automatic re-weighting of categories to zero
Hospitals that were impacted by hurricanes Irma, Harvey and Maria or other natural disasters will automatically have their Quality, ACI and IA categories re-weighted to zero percent in 2017.
If a hospital would also like this same treatment in 2018, they must submit a hardship exception application by December 31, 2018.

11. Virtual Groups
New this year is the concept of Virtual Groups, which will allow individual clinicians and small groups to come together to form one virtual group that can report together. Clinicians do not need to be in the same area of the country or be in a similar specialty to be in the same group. All members of the virtual group must be Eligible Clinicians either at an individual level or a group level.

12. Improvement Bonus
Another nice little bonus will be awarded to any clinicians whose Quality or Cost score has improved over last year (pending there is enough data for comparison). You can receive up to 10 bonus points in the Quality category and one additional bonus point in the Cost category. Keep in mind, CMS will figure an improvement score only when there's sufficient data to measure improvement. So make sure to submit your data for 2017!
13. Complex Cases Bonus
An additional five bonus points may be added to the clinician’s final score based on the medical complexity of patients they see.
ON-DEMAND WEBINAR:
MIPS 2019: A REVIEW OF THE PROGRAM REQUIREMENTS
What’s in store for MIPS year three?
In this free educational webinar, we discuss who is eligible for the MIPS program in 2019 and what’s required for successful completion of the program. We also outline strategies that will help your providers gear up for their best reporting year yet.
Here’s what's covered in this webinar:
- Changes made in the 2019 final rule for the Quality Payment Program
- Reporting requirements for MIPS
- How the final score is calculated
- Best practices for preparing your clinicians for a successful quality reporting year
Speaker info:
Denise Scott
Director of Ambulatory Service
Medisolv, Inc


.png?width=352&name=2026%20Quality%20Reporting%20Deadlines%20Guide%20(1).png)



Comments