An Overview of the 2019 Quality Payment Program: MIPS vs Advanced APMs
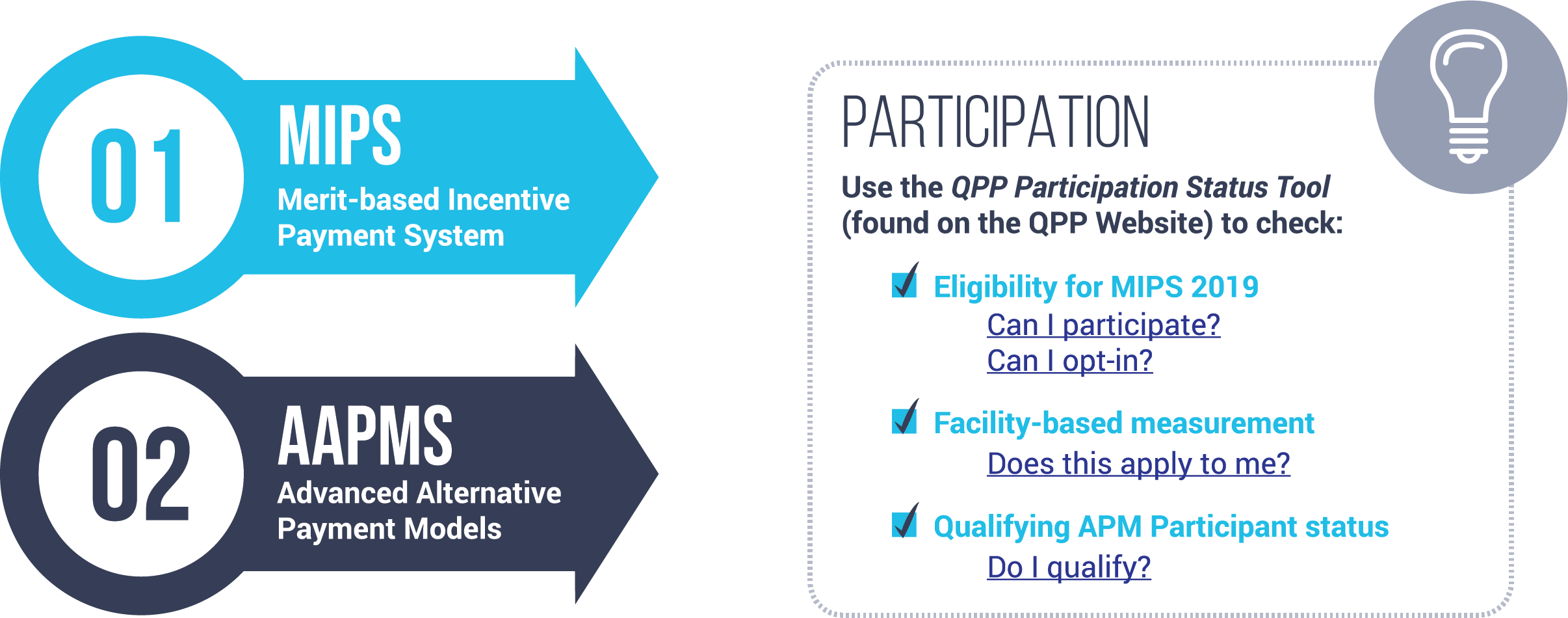
There are two different tracks to the Quality Payment Program: MIPS and Advanced APMs. By now, we are all pretty familiar with the terms. But did you know that if you participate in an APM (such as an ACO) you may still be required to report to MIPS?
Preparing for a successful QPP participation can be challenging, especially if you wait until the last minute to do your research and make a game plan. Keep in mind that the reporting period for QPP has already begun.
In this post we give a simple overview of the Quality Payment Program and help to explain the difference between the two different tracks.
Note: CMS made a few changes to your 2019 MIPS requirements in response to COVID-19. Changes are noted below. Read our blog, to learn more about the overall changes to quality reporting in response to COVID-19.
What is the Quality Payment Program?
The History of QPP
In 2015, Congress passed a bill for Medicare payment reform that is designed to lower healthcare costs and improve the quality of patient care.
From the Medicare Access and CHIP Reauthorization Act (MACRA) legislation was born the Quality Payment Program.
The Quality Payment Program in 2019
The Quality Payment Program combined previous provider reporting programs (PQRS, Meaningful Use and Value-Based Modifier) into one comprehensive program.
There are two ways to participate in the Quality Payment Program
Who is Eligible for MIPS?
The following clinician types are eligible for MIPS:

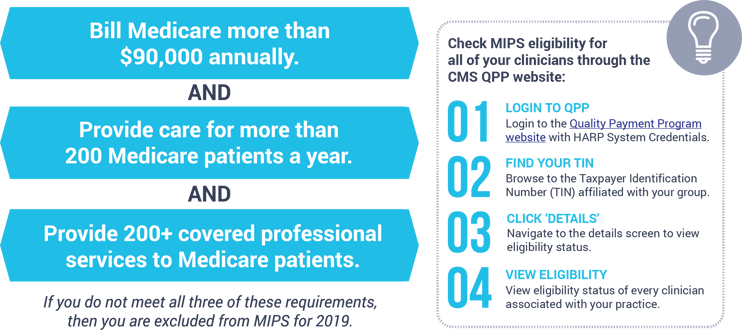
It’s not just a title that makes you eligible for this program. You must also meet the three requirements below.
MIPS Incentive Payments
If you are eligible and do not score at least 30 points, you can lose up to -7% of your Medicare fee reimbursement to your 2021 payments. On the flip side you can earn up to 7% PLUS bonus money for the best performers.
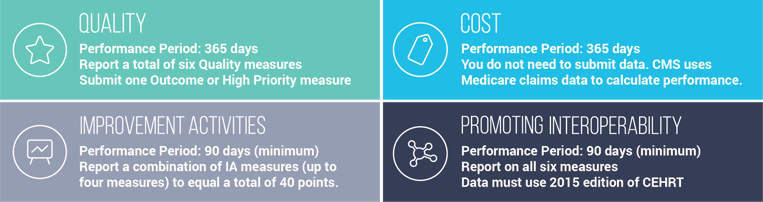
MIPS Performance Categories
The four MIPS performance categories and weights are as follows:

MIPS Category Requirements
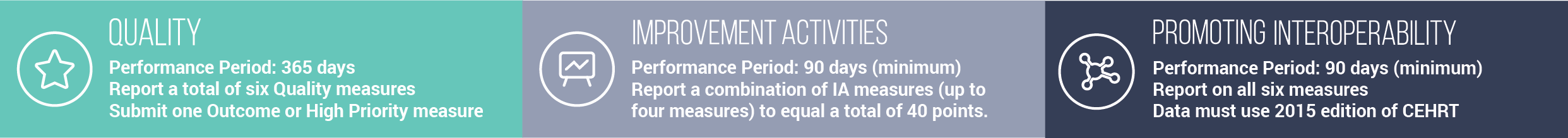
To full participate in MIPS, you must collect and submit the following:
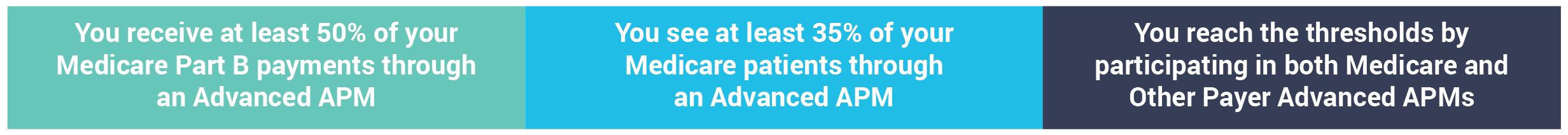
Who is Eligible for Advanced APMs?
To be eligible for this path you must be a Qualifying Participant in an Advanced APM. To be a qualifying participant you must meet the following:
Advanced APM Incentives
If you qualify as an Advanced APM Qualifying Participant (QP) you may earn 5% incentive money added to your 2021 Medicare fee reimbursement.
Advanced APM Requirements
Unlike MIPS, if you are found to be a QP for an Advanced APM you do not have any additional submission requirements. CMS recognizes the data you submit to your Advanced APM as equivalent to the data you would have been required to submit as a part of MIPS.
If you are in an APM you may still need to report MIPS! Only Advanced APMs do not need to submit to MIPS.
Who is Eligible for MIPS APM?
If you meet the MIPS eligibility requirements listed above and you are in an APM that is not one of the Advanced APMs, then you must still report to the MIPS program.
MIPS APM Incentives
Your incentives are the same as the general MIPS participants. You may gain up to 7% PLUS bonus money for good performance and lose up to -7% for poor performance.
MIPS APM Categories
If you’re eligible for MIPS and participate through a MIPS APM, the categories and weights are:
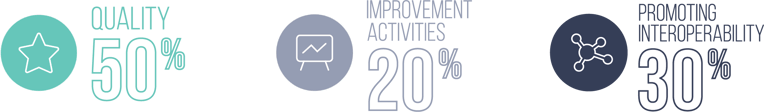
*The Cost category is not scored for MIPS APM participants.
MIPS APM Category Requirements
To full participate in MIPS, you must collect and submit the following:
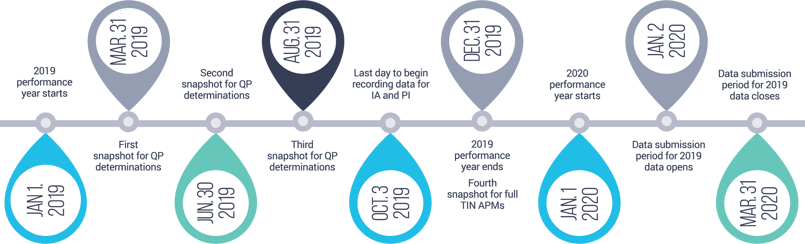
MIPS 2019 Deadlines
|




.png?width=352&name=BlogImage_2025%20APP%20Reporting%20Requirements%20for%20ACOs%20(2).png)
Comments