[PART 1] Understanding MIPS 2018
![[PART 1] Understanding MIPS 2018](https://blog.medisolv.com/hs-fs/hubfs/UNDERSTANDING-Mips-2018.jpg?width=900&height=600&name=UNDERSTANDING-Mips-2018.jpg)
In this first post of our four-part series on MIPS 2018, we begin with an understanding of the basic structure of the MIPS program. We review where it came from and the general things you need to know about how the program works.
The Structure of the Quality Payment Program
The Quality Payment Program was created as a result of the billed passed by Congress called the MACRA Act of 2015. MACRA stands for Medicare Access and CHIP Reauthorization Act (only in health care and politics would they shove an acronym inside an acronym). The MACRA legislation was intended to change the way in which providers are paid. The goal of the program, like many programs nowadays, is to focus on quality versus quantity.
This legislation also required that CMS set up two tracks. The MIPS track combined several provider reporting programs (PQRS, Meaningful Use and Value-Based Modifier) into one comprehensive program. If you are eligible and report to this program, you are either subject to a penalty or a payment increase based upon the data that you submit.
The Advanced Alternative Payment Model (APM) track lets practices earn more for taking on some risk related to patients’ outcomes. If you are a part of the Advanced APM track, you automatically receive a 5% increase to your Medicare reimbursement which would be effective in 2020 Medicare fee schedule.
People tend to confuse being a part of an ACO (Accountable Care Organization) as automatically being eligible for the Advanced APM track. This is not necessarily the case. If you are a part of an ACO, you may still be required to report to the different categories of the MIPS program. Only Advanced APMs are eligible to report under the second track.
Here are some examples of Advanced APMs for 2018.
- Comprehensive Primary Care+ Model
- Comprehensive ESRD (CEC) Care Models (two-sided risk)
- Comprehensive Care for Joint Replacement Model (CEHRT Track)
- Medicare ACO Track 1+ Model
- MSSP ACO Tracks 2 & 3
- Next Generation ACO Model
- Oncology Care Model (two-sided risk)
- Vermont Medicare All-Payer ACO Model
Now, we are going to focus on the requirements for the MIPS track below.
Who is Eligible for MIPS in 2018
In the second year of the program, the eligibility requirements have changed. The actual clinicians who are eligible to report are the same. The Eligible Clinicians are:
- Physician (including doctors of medicine, doctors of osteopathy, osteopathic practitioners, doctors of dental surgery, doctors of dental medicine, doctors of podiatric medicine, doctors of optometry, and chiropractors)
- Physician Assistant
- Nurse Practitioner
- Clinical Nurse Specialist
- Certified Registered Nurse Anesthetist
In 2019, they plan to expand the Eligible Clinicians to include:
- CNMs
- LICSWs
- Clinical Psychologists
- Physician Therapists Occupational Therapists
- Audiology
- Speech
- RDs
In addition to being one of these Eligible Clinicians, you must also have billed Medicare $90,000 or more in allowable charges and provided care for more than 200 Medicare beneficiaries. If you don’t meet both of these requirements, you are not eligible. Also, you must not be in your first year of Medicare.
This is a change from last year where Eligible Clinicians had to bill Medicare only $30,000 in allowable charges and provided care for only 100 or more beneficiaries. So, does this mean you’re excluded this year? Well maybe. The change mostly impacts solo practitioners. Many physicians are reporting as a part of a group. Once your group exceeds that $90,000 and 200 beneficiaries limit, your group has to report.
2018 MIPS Reporting Options
Speaking of reporting, there are a couple of different ways that you can report to the MIPS program in 2018. You can report as an individual Eligible Clinician or as a group of Eligible Clinicians (made up of two or more Eligible Clinicians), or, new this year, you can report via a Virtual Group.
Virtual Groups are made up of individual or groups of Eligible Clinicians that come together virtually to form one submission group. Clinicians do not need to be in the same area of the country or be in a similar specialty to be in the same group. One caveat, all members of the virtual group must be Eligible Clinicians either at an individual or group level. These groups had to have registered with CMS by December 31 of 2017 to report as a virtual group in 2018.
Once the 2017 MIPS reporting year has ended, CMS will update their website with 2018 eligibility data. At that point you can head over to the Quality Payment Program website and, using a clinician’s NPI, see if that clinician is eligible. Again, just be aware if the clinician is reporting as an individual, then they are identified by CMS using their NPI. But if the clinician is a part of a group, then CMS identifies the group as eligible using the Tax ID (TIN) for the group.
MIPS Payment Adjustments for 2018
The MIPS reporting year started on January 1, 2018 and closes on December 31, 2018. All data must be submitted by April 2, 2019.
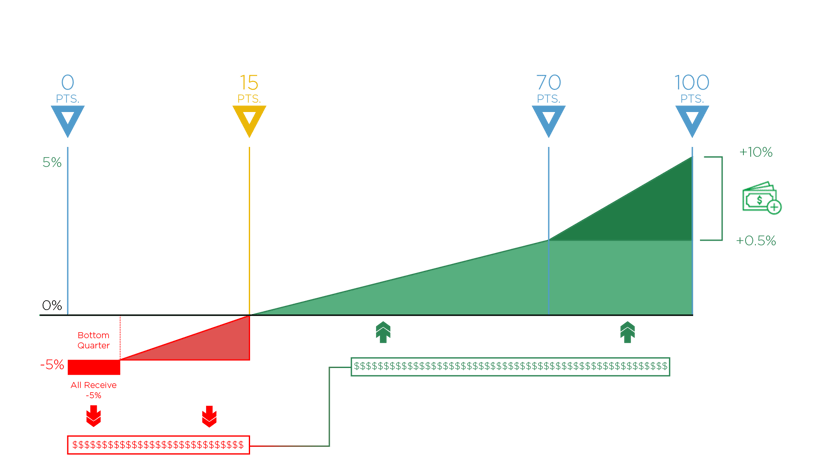
The payment adjustments are moving ahead as required by law. For 2018, you have a maximum reduction of -5%. On the flip side, the maximum positive adjustment is up to 5%. But keep in mind the MIPS program is a budget neutral program. This means only the funds that are received from the negative adjustment will be distributed to those who achieve the positive adjustment. So, it’s difficult to say how much positive adjustment you may receive because it is not known how many people will receive the negative adjustment to their Medicare reimbursement until it's all said and done. These adjustments will impact your 2020 Medicare reimbursement.
In order to be on the positive side of the adjustment, you must reach a score of 15 points (the performance threshold). If you score at least 15 points, you will avoid a penalty. That’s up from only three points last year. If you score less than 15 points, you could get a reduction. And the bottom quarter of the worst performers will receive the full -5% reduction.
If you are able to score above 70 points, then you’ll be eligible for even more cash. CMS set aside $500 million additional dollars to fund the Exceptional Performance Bonus which would be applied in addition to any positive adjustments you receive.
Here is a visual of how the payment adjustment works to make it a little easier to understand.
MIPS Categories 2018
In 2018, all four categories of MIPS count toward your final score. The four categories are Quality, Advancing Care Information, Improvement Activities and Cost.
Each category counts toward a certain percentage of your overall score. This is the first year that the Cost category counts toward your total score. Cost is weighted at 10% which in turn lowered the Quality category weight to 50%.

MIPS Reporting Options
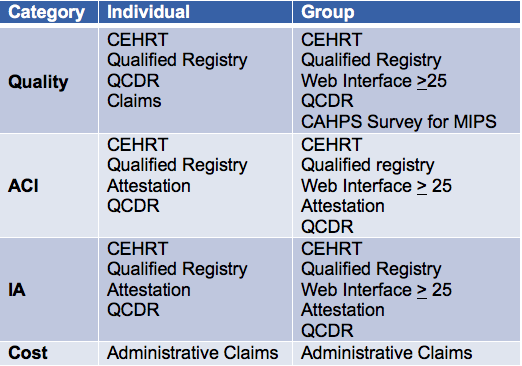
Your methods of reporting to MIPS have not changed from last year. Within each category you have different reporting methods available to you. First, let’s review the reporting methods.
- Using CEHRT (Certified EHR Technology): This method uses a vendor like Medisolv to submit your measures. Vendors must be certified to the 2014 or 2015 Edition of CEHRT
- Qualified Registry: This method also uses a vendor like Medisolv to submit your measures. Registries just have different measures that they are able to submit to CMS.
- Qualified Clinical Data Registry (QCDR): QCDRs are similar to Qualified Registries except they are able to create their own measures that they can submit to CMS. This is only really needed for highly specialized clinicians that can’t find eCQMs or Registry measures that will work for them.
- CMS Web Interface: If your group has more than 25 Eligible Clinicians, you can submit your measures using the CMS Web Interface. You must inform CMS by June 30, 2018.
- Claims: This is the normal method of submitting administrative claims.
Here is a chart showing you which reporting method you can and cannot use for each category. Notice that it changes depending on whether you are submitting as an individual or a group.
In the following weeks, we will dive deeper into each of these categories. We will include category requirements and tips for success.
on-demand WEBINAR:
MIPS 2019: A REVIEW OF THE PROGRAM REQUIREMENTS
What’s in store for MIPS year three?
In this free educational webinar, we discuss who is eligible for the MIPS program in 2019 and what’s required for successful completion of the program. We also outline strategies that will help your providers gear up for their best reporting year yet.
Here’s what's covered in this webinar:
- Changes made in the 2019 final rule for the Quality Payment Program
- Reporting requirements for MIPS
- How the final score is calculated
- Best practices for preparing your clinicians for a successful quality reporting year


.png?width=352&name=2026%20Quality%20Reporting%20Deadlines%20Guide%20(1).png)



Comments