2022 IQR and PI Program Changes: A Summary from the IPPS Final Rule

CMS released their 2022 IPPS Final Rule and there was a lot in it. The biggest takeaway from this ruling is that CMS is moving toward all digital measurement at rapid speed. They are ramping up eCQM and hybrid measure requirements and outlining definitions of dQMs (digital quality measures).
In this article we are covering the changes to the Hospital Inpatient Quality Reporting (IQR) and Promoting Interoperability (PI) programs.
For more information about dQMs read What are dQMs?
Let’s take a look at what CMS has in store for us in 2022.
First, some resources:
Hospital IQR Program Changes
Let’s start with the IQR program.
New Measures for This Year
There are two new measures that you must report for this year (2021). The reporting period is October 1, 2021 – December 31, 2021.
1. Maternal Morbidity structural measureThis is a structural measure meant to address the US problem with maternal mortality. The rate of maternal mortality rose from 17 deaths per 100,000 live births in 1990 to 26 deaths per 100,000 live births in 2015. CMS found one of the main factors to be inconsistent obstetric practice.
This measure was developed to see how many hospitals participate in a State or national Perinatal Quality Improvement Collaborative and within that collaborative implement patient safety practices or bundles.
To report this measures, your hospital will need to answer a two-part question: “Does your hospital or health system participate in a Statewide and/or National Perinatal Quality Improvement Collaborative Program aimed at improving maternal outcomes during inpatient labor, delivery and post-partum care, and has it implemented patient safety practices or bundles related to maternal morbidity to address complications, including, but not limited to, hemorrhage, severe hypertension/preeclampsia or sepsis?”
Hospitals must submit responses once a year through QualityNet.
2. COVID-19 Vaccination Coverage among Health Care Personnel (HCP) measureThis is a process measure meant to incentivize and track HCP vaccination in hospitals. CMS wants to track how many HCPs are vaccinated. They are going to publicly report that information on Care Compare.
To report this measure, hospitals would collect the denominator (number of HCP eligible to work in the hospital for at least one day of the reporting period) and the numerator (all those in the denominator who received a completed vaccine). This measure is reported on a quarterly basis starting with the Oct - Dec 2021 timeframe and then continuing throughout 2022. Hospitals self-select one week of each month of the reporting quarter and submit the data to NHSN.
The CDC will then average the data from the three submitted weeks of the quarter and publicly report it on Care Compare starting in October 2022.
New Hybrid Measure for Next Year
CMS is adding a new Hybrid measure to the list of available measures in 2022. The Hybrid Hospital-Wide All-Cause Risk Standardized Mortality (Hybrid HWM) measure is available for voluntary reporting from July 1, 2022 – June 30, 2023 and then mandatory reporting starting July 1, 2023.
This hybrid measure is similar to the Hybrid Readmission (HWR) measure in the fact that it uses almost all of the same Core Clinical Data Elements (CCDE) and the exact same linking variables. This measure, however, captures mortality within 30 days of hospital admission for most conditions or procedures.
To report this measure, hospitals must submit a QRDA-I file with the CCDE and linking variables within three months of the end of the reporting period (i.e. October 1).
For more information about the Hybrid measure read What is the Hybrid Readmission Measure?
For HWM specification information visit the CMS website.
New eCQMs for 2023
CMS added two new eCQMs to the list of available measures in 2023. They are not required as of yet, just available.
They are:
1. Hospital Harm-Severe Hypoglycemia eCQM
2. Hospital Harm-Severe Hyperglycemia eCQM
CMS found that the rate of severe hypo and hyperglycemia vary across hospitals which indicates there is room for improvement.
The Hypoglycemia eCQM identifies patients who had a severe hypoglycemic event (glucose result of less than 40 mg/dL) within 24 hours of an administration of an antihyperglycemic agent.
The Hyperglycemia eCQM identifies the number of days a patient had a severe hyperglycemic event (glucose result of >300 mg/dL) during the visit and it was proceeded by two consecutive days where at least one glucose value was >=200 mg/dL.
Retiring eCQMs in 2024
CMS is retiring the following three measures in 2024:
- Exclusive Breast Milk Feeding (PC-05)
- Admit Decision Time to ED Departure Time for Admitted Patients (ED-2)
- Discharged on Statin Medication eCQM (STK-06)
Other things to note
One other thing to note for eCQM submission in the IQR program is that hospitals are required to use certified technology that is updated to the 2015 Edition Cures Update for all eCQMs and hybrid measures.
Hospital PI Program Changes
Moving on to the Promoting Interoperability program.
EHR Reporting Period Minimum
Hospitals may continue to report a continuous 90-day period for 2022 and 2023 but in 2024, hospitals must report a minimum of a continuous 180-day period.
PDMP Reporting and Points
CMS will continue the Electronic Prescribing Objective’s Query of PDMP measure as optional in 2022. But they are increasing the number of bonus points you can get to 10 points.
Adding new HIE Bi-Directional Exchange measure
CMS is providing hospitals an optional new measure that is worth 40 points in 2022. This one measure could be submitted instead of reporting on the two existing HIE objective measures: the Support Electronic Referral Loops by Sending Health Information measure and the Support Electronic Referral Loops by Receiving and Reconciling Health Information measure.
Reporting on four Public Health and Clinical Data Exchange Objective measures
In the past, hospitals were required to report any two measures from their choice of 6 measures:
- Syndromic Surveillance Reporting
- Immunization Registry Reporting; Clinical Data
- Registry Reporting
- Electronic Case Reporting
- Public Health Registry Reporting
- Electronic Reportable Laboratory Result Reporting
In 2022, hospitals must submit all four of these measures:
- Syndromic Surveillance Reporting
- Immunization Registry Reporting; Clinical Data
- Electronic Case Reporting
- Electronic Reportable Laboratory Result Reporting
Adding a new measure to the Protect Patient Health Information objective
In 2022, hospitals have a new measure to report. They must attest to having completed an annual assessment of SAFER Guides.
SAFER (Safety Assurance Factors for EHR Resilience) Guides are a series of nine user guides that help hospitals optimize the safety and safe use of their EHR.
The SAFER Guides are:
|
Foundational Guides |
1. High Priority Practices |
|
Infrastructure Guides |
3. System Configuration |
|
Clinical Process Guides |
5. Patient Identification |
Each year hospitals must conduct an annual self-assessment of all nine SAFER Guides (available at https://www.healthit.gov/topic/safety/safer-guides). This measure is required next year but it won’t be scored. So, you can answer “yes” or “no” with no consequence.
Removing two attestation statements from the prevention of information blocking requirement.
CMS is removing Statement 2 and Statement 3 from the prevention of information block requirement.
Increasing the score threshold
CMS is increasing the minimum required score for the Promoting Interoperability program from 50 points to 60 points (out of 100) in order for a hospital to be considered a meaningful EHR user.
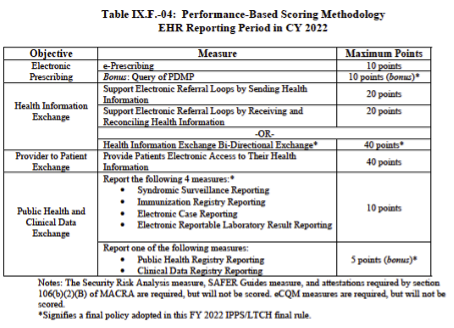
Here is the measure list for 2022 and the maximum points you can achieve.
Other things to note
Two other things to note here. The PI program is adopting the same two eCQMs (mentioned above) in 2023 and removing the same three eCQMs (mentioned above) in 2024 to align with the IQR program.
Also, CMS decided not to modify the Provide Patients Electronic Access to Their Health Information measure. They were proposing to require hospitals to make patient health information available to a patient indefinitely (with data from January 1, 2016 and after), but decided against it after too much push back.
This is a very high-level summary of the changes. We will be rolling out more information on each of these subjects this year. Our client education on the changes to requirements and measure specification updates begins in early fall.
If you’d like to learn more about how Medisolv can help your organization with your IQR and PI program needs (especially eCQMs and hybrid measures), please contact us today to get started.
Stay Ahead of the Quality CurveMedisolv Can Help
Here are some resources to help you get started:
|






Comments