2024 APP Reporting Requirements for ACOs
The Quality Payment Program (QPP) has allowed large organizations to use the CMS Web Interface reporting method to complete MIPS requirements since the program launched in 2017. This gave these organizations the option to report a sampling of 248 patients (selected by Medicare Part B claims) across all their practices. CMS will completely sunset the CMS Web Interface reporting option by 2025.
In 2025, all MSSP ACOs must report either eCQMs, CQMs, or Medicare CQMs across all of their practices for 365 days of the year.
Figuring out data aggregation, de-duplication, and comprehensive performance review before 2025 is the key to your success. Below is a summary of your 2024 APP requirements.
|
Learn How Medisolv Helps Hospitals Navigate QPP Changes in 2024 |
APM Performance Pathway (APP) Reporting Requirements
There are three reporting frameworks available in the Quality Payment Program, but MSSP ACOs can only submit to one, the APM Performance Pathway (APP) reporting framework.
Also read: A comparison of the 2024 requirements for all three reporting frameworks.
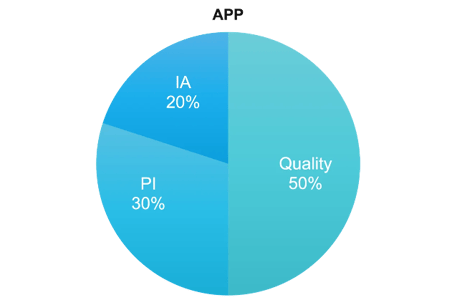
APP Framework Category Weights
For the APP framework there are three categories, Quality, Promoting Interoperability, and Improvement Activities. Cost is weighted at 0%.
Defining QPP Collection Types
Collection types are the way you report the data to CMS. You can think of them like measures. There are six collection types in 2024.
- eCQMs (Electronic Clinical Quality Measures)
- MIPS CQMs (previously called Registry measures)
- Medicare CQMs (new for 2024)
- QCDR measures (Qualified Clinical Data Registry)
- Medicare Part B Claims measures
- CAHPS for MIPS survey
- CMS Web Interface measures (<< not available in 2025)
APP Framework: Quality Category Requirements
Category weight: 50% of total score
Performance Period: 365 days
Requirements:
Option 1 (<<your only option in 2025)
- Submit 3 eCQMs, CQMs, or Medicare CQMs
- You may use a combo of collection types (eCQMs or CQMs)
- Two administrative claims measures are calculated automatically by CMS
- CAHPS for MIPS survey
Option 2 (<<not available in 2025)
- Submit 10 CMS Web Interface measures
- Report data for 100% of assigned Medicare beneficiaries identified by CMS (248 cases)
- Two administrative claims measures are calculated automatically by CMS
- CAHPS for MIPS survey
Option 3 (<<not available in 2025)
- Submit 3 eCQMs, CQMs, or Medicare CQMs AND 10 CMS Web Interface measures
- You may use a combo of collection types (eCQMs or CQMs)
- CMS will give you the highest score out of the two options when you submit both
- Two administrative claims measures are calculated automatically by CMS
- CAHPS for MIPS survey
Measure list:
Quality Measures
- eCQMs/CQMs/Medicare CQMs
- Quality ID: 001 Diabetes: Hemoglobin A1c (HbA1c) Poor Control
- Quality ID: 134 Preventive Care and Screening: Screening for Depression and Follow-up Plan
- Quality ID: 236 Controlling High Blood Pressure
- CMS Web Interface Measures
- Quality ID: 001 Diabetes: Hemoglobin A1c (HbA1c) Poor Control
- Quality ID: 134 Preventive Care and Screening: Screening for Depression and Follow-up Plan
- Quality ID: 236 Controlling High Blood Pressure
- Quality ID: 318 Falls: Screening for Future Fall Risk
- Quality ID: 110 Preventive Care and Screening: Influenza Immunization
- Quality ID: 226 Preventive Care and Screening: Tobacco Use: Screening and Cessation Intervention
- Quality ID: 113 Colorectal Cancer Screening
- Quality ID: 112 Breast Cancer Screening
- Quality ID: 438 Statin Therapy for the Prevention and Treatment of Cardiovascular Disease
- Quality ID: 370 Depression Remission at Twelve Months
Claims Measures
- Hospital-Wide, 30-Day, All-Cause Unplanned Readmission (HWR) Rate for MIPS Eligible Groups.
- Clinician and Clinician Group Risk-standardized Hospital Admission Rates for Patients with Multiple Chronic Conditions
CAHPS for MIPS Survey measure
APP Framework: PI Category Requirements
Category weight: 30% of total score
Performance Period: 180 days
Requirements:
Submit the required measures (measure list below)- Attest to these two measures: Prevention of Information Blocking and ONC Direct Review
- Collect your data in EHR technology certified to the 2015 Edition or 2015 Cures Edition Update, or a combination of both
- Provide your EHR’s CMS Identification code from the Certified Health IT Product List (CHPL)
- Conduct or review a security risk analysis on your CEHRT functionality on an annual basis
- Attest to conducting an annual assessment of the Safety Assurance Factors for EHR Resilience Guides (SAFER Guides)
Measure List:
Promoting Interoperability Measures
- E-Prescribing
- Query PDMP
- Sending Health Information AND
- Receiving and Recording Health Information OR
- HIE Bi-Directional Exchange OR
- Enable Exchange under TEFCA
- Provide Patients Electronic Access to Health Information
- Electronic Case Reporting
- Immunization Registry
- Public Health Registry
- Syndromic Surveillance
- Clinical Data Registry
Other Considerations
You must submit the PI Category:
- At an aggregate level on behalf of 100% of your Eligible Clinicians
OR - 100% of your Eligible Clinicians may submit as an individual or part of a group submission separately.
By 2025 ACOs must have all their practices off of paper and on Certified EHR Technology (CEHRT).
APP Framework: IA Category Requirements
Category weight: 20% of total score
Requirements:
All APM Entities reporting through the APP Framework will be automatically assigned a score of 100% which is applied to all Eligible Clinicians reporting through their APM Entity.
Achieving Shared Savings in 2024
In 2024, for an MSSP ACO to get the maximum shared savings they must achieve a quality performance score that is greater than or equal to a certain percentile of the benchmark and meet the Shared Savings Program Quality Performance Standard.
Shared Savings
To get the maximum shared savings for your ACO you must:
Report ALL measures in the APP measure set
AND
Achieve the Quality Performance Standard
CMS has implemented a sliding scale to give ACOs some percentage of the Shared Savings (not max) if they don’t meet the quality performance standards but do achieve a quality performance score equivalent to or higher than the 10th percentile of the performance benchmark on at least one of the four outcome measures.
Maximize Your Shared Savings
Quality Performance Standard
- Report eCQMs/CQMs
- Achieve a score = > 10th percentile on 1 outcome measure
- Achieve a score = > 40th percentile on at least 1 of the remaining measure
OR
Health Equity-Adjusted score of => 40th percentile across ALL quality performance scores
Quality Performance Standard
CMS will calculate 2024 and 2025 benchmarks for the Medicare CQMs based on performance period benchmarks. They will transition to historical benchmarks in 2026 and subsequent years.
This means that ACOs will not know the Medicare CQM benchmarks during the performance period.
CMS is NOT extending the eCQM/MIPS CQM reporting incentive to Medicare CQMs.
CMS finalized the use of historical data to establish the 40th percentile MIPS Quality performance category score used for the quality performance standard.
That means you would know what the Quality Performance Standard percentile is BEFORE the performance year starts.
40th Percentile MIPS Quality Performance Category Scores Used in the Calculation of the PY 2024 Historical MIPS Quality Performance Category Score
|
Performance Year |
40th Percentile of the MIPS Quality Performance Category Score |
|
2020 |
75.59^ |
|
2021 |
77.83^ |
|
2022 |
77.73^ |
|
2023 |
Skipped due to 1-year lag |
|
2024 |
77.05 |
^ PY 2020 through PY 2022 40th percentile scores are based on performance period data
Important Dates
January 1, 2024
The start date to track 365 days of Quality and Cost category measures.
April 1, 2024
Registration opens for CMS Web Interface, CAHPS for MIPS Survey, and MVP selection.
July 4, 2024
The last day to start measures in the Promoting Interoperability category to meet the minimum of 180 continuous days.
October 2, 2024
The last day to start Improvement Activities to meet the minimum requirement of 90 continuous days.
March 31, 2025
The last day to submit all of your performance data.
Data Completeness Requirements
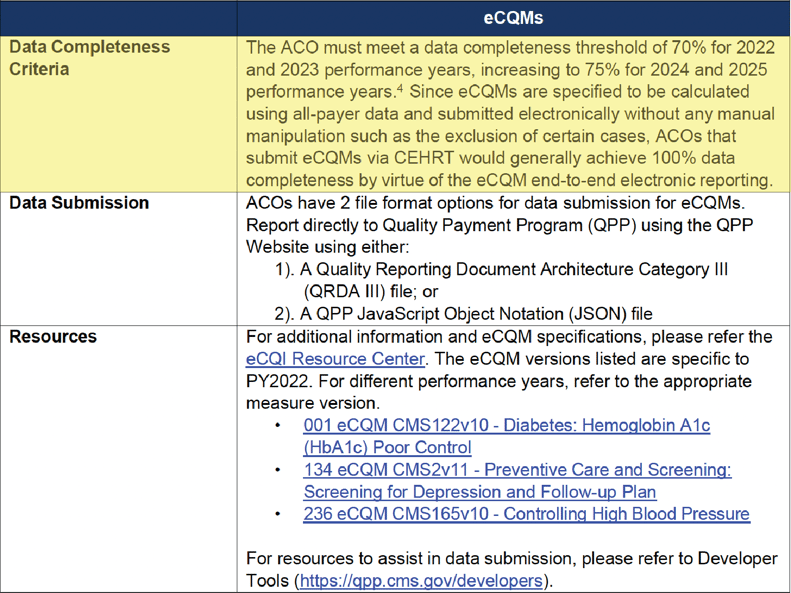
There has been SO MUCH discussion on this topic. I once watched an ACO representative grill a CMS representative in a live panel discussion for no less than 20 mins on this topic. I think we all left even more confused. CMS attempted to make it clearer by releasing a new guide to Data Completeness that further validates the 100% of eligible patients. They make it very clear that no one can be excluded from the Denominator population.
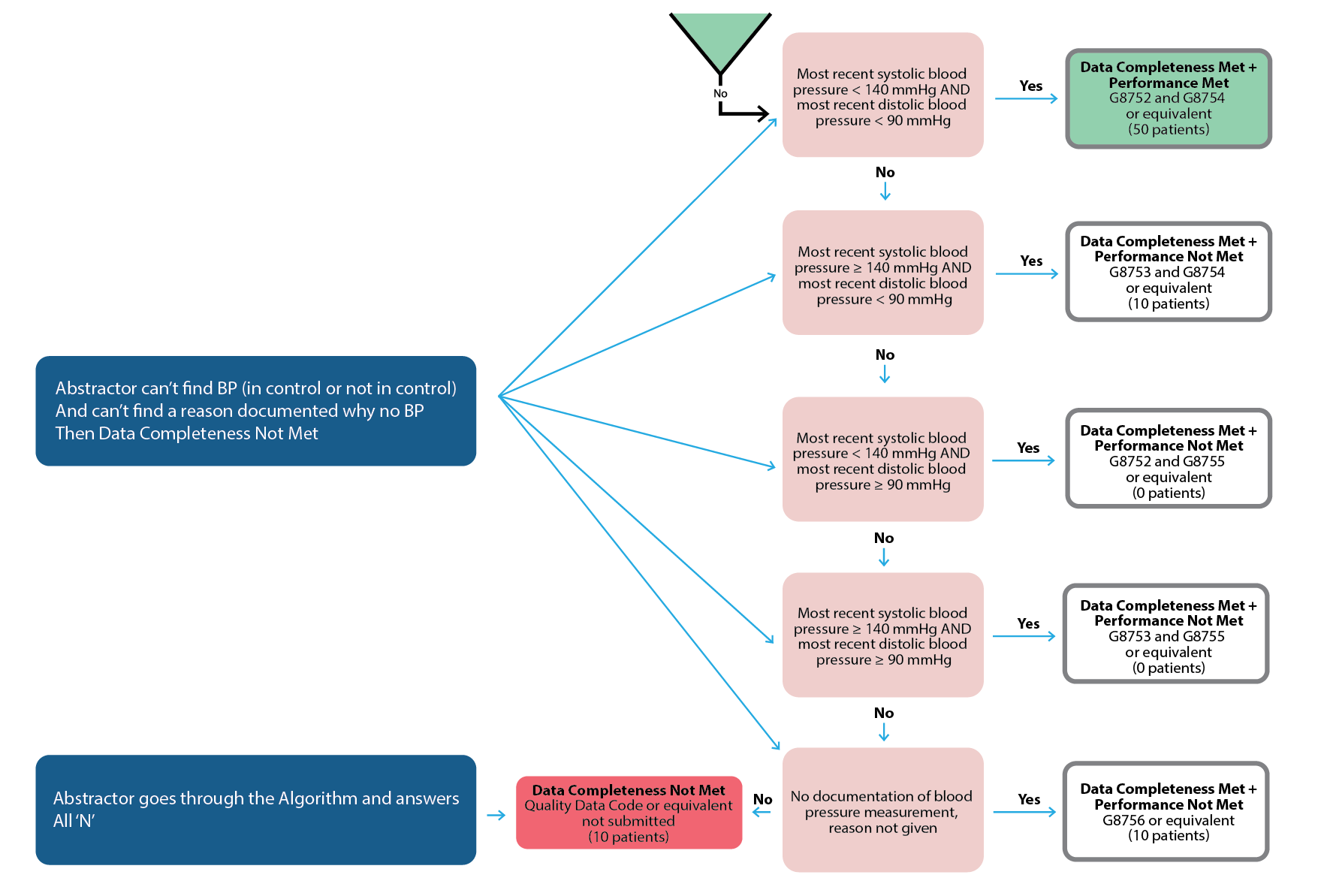
An ACO must submit their entire “universe” of patients. None of your practices can be excluded based on populations. The data completeness threshold really would only be applicable in a MIPS CQM situation and even in that situation you still must have the entire universe of practices/patients and only achieve 70% completeness on the denominator patients.
Take a look at pages six and eight of the APP guidance document here.
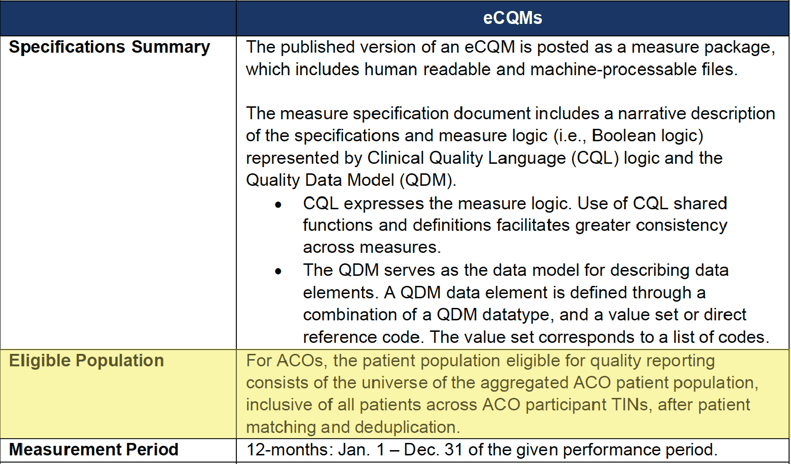
eCQM Data Completeness Criteria Summary
MIPS CQM Data Completeness Criteria Summary
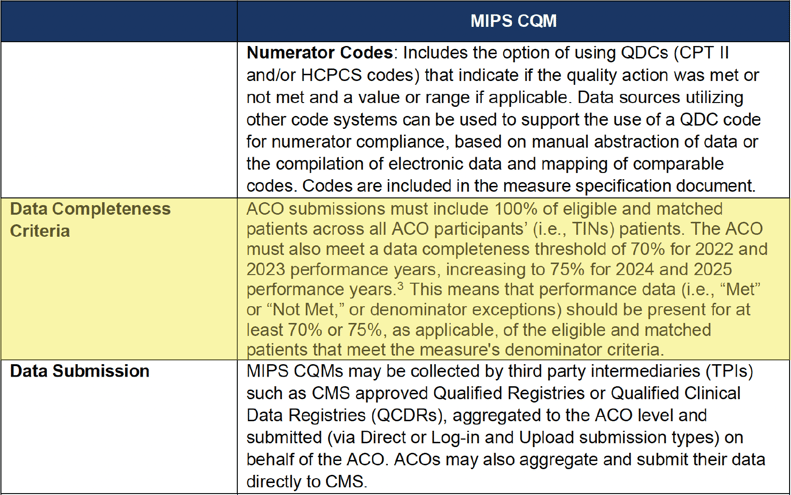
When is the data completeness threshold applicable?
It’s an unlikely scenario. But in some cases, an abstractor can't find the documentation that’s required by the measure. In this red scenario below an abstractor answers “no” to algorithm questions for more than 30% of cases.
How to Get Started With eCQM/CQM Reporting
ACOs must learn to juggle multiple, disparate EHRs and data collection methodologies. Developing a cohesive data aggregation system is going to be a major undertaking. Your senior leadership, quality management, and information technology teams need to start planning what that looks like for your ACO now.
The most important thing you can do right now is understand what your data landscape looks like. Here are a couple of questions you should know.
- Which practices are on which EMRs? Make a list.
- How many instances of each EMR vendor do you have?
- Do you have any practices still on paper charts? (<<If so, you cannot report to CMS.)
- How many practices are on less common EMRs?
- Can every single practice generate a QRDA I file (<<Applicable for eCQMs. Especially focus on those practices with less common EMRs.)
- Do you capture CPT II (G codes) in a database for all practices? (<<Applicable for MIPS CQMs.)
This information will help you to choose whether you want to submit eCQMs or MIPS CQMs. It will also inform you as to whether or not you have to set up conversations with any practices not able to provide your group with what you need.
How Long Will the Data Acquisition Process Take?
This is completely dependent upon your organization set up. For most of our clients, we tell them to estimate a 6–8-month implementation time before you start to see any meaningful data.
Final Thoughts: Don’t Wait
It's in your best interest to start looking at your data through the all-patients, all-payers, all-practices lens now. It is the key to unlocking so many other patient care goals for you, including improving population health, reducing health care costs, and advancing health equity. For too long, the CMS Web Interface had made quality reporting a box that organizations had to check. It’s time now for organizations like yours to lead the charge to elevate the role of quality data in patient care. Together, we have the power to put quality data to good use.
More Resources to Prepare Your ACO For What’s Next
At Medisolv, we offer so much more than quality software and start-to-finish submissions management. We’re the quality improvement partner committed to deciphering and anticipating CMS’s regulatory changes for you—so that you can keep your organization ahead of the curve.
Check out some of our additional resources now:
- eBook: CMS Web Interface Transition Guide
- Article: 2024 QPP Requirements
- On-Demand Webinar: Preparing your ACO for APP Reporting
Medisolv Can HelpAlong with award-winning software, each client receives a dedicated Clinical Quality Advisor that helps you with your technical and clinical needs. We consistently hear from our clients that the biggest differentiator between Medisolv and other vendors is the level of one-of-one support. Especially if you use an EHR vendor right now, you’ll notice a huge difference.
|

.png?width=352&name=2026%20Quality%20Reporting%20Deadlines%20Guide%20(1).png)



Comments