2024 QPP Requirements

The Quality Payment Program has undergone some major changes over the last several years and CMS has signaled that they intend to further modify the program in the years to come. It's hard to keep all the requirements straight. In this article, we will cover the major themes that came out of the recent final ruling, review the base requirements for all participants and then review the individual requirements according to a clinician’s participation status.
Major Theme Changes
There are three major themes to the changes CMS unfolded as a part of the 2024 PFS Proposed Rule.
Theme 1: MSSP ACOs must start reporting using eCQMs, CQMs, or Medicare CQMs. CMS did not extend the deadline for transitioning away from CMS Web Interface measures. That means by 2025, everyone must report Quality measures as either eCQMs, CQMs, or Medicare CQMs.
Also see: eCQM vs CQM vs Web Interface: Understanding the Difference
Theme 2: Subgroup reporting by specialty type is here. CMS expanded their reporting framework called MIPS Value Pathways (MVPs). MVPs include measures that are for specific specialty groups (like rheumatologists). CMS added five more MVPs, bringing the total to 16 different MVPs a group could use to report in 2024. Full sub-group reporting is optional until 2026, when it becomes mandatory (if you choose to report this framework).
Also see: The 2024 MVP Reporting Bundle
Theme 3: The end of Traditional MIPS is hovering like a specter above us. CMS didn't commit to it, but they haven’t officially backed off their statement that says they will retire the Traditional MIPS reporting framework at the end of 2027, which would mean everyone must report under the MVP reporting framework (subgroup reporting by specialty type required) or be involved with an APM Entity (such as an ACO) and report through the APM Performance Pathway (APP) framework.
Let’s dive into the details.
Participation Eligibility
CMS puts Eligible Clinicians into one or more categories.
CMS puts Eligible Clinicians into one or more categories.
To find out your participation framework you must check your eligibility on the QPP website. Enter the provider NPI to determine eligibility.
- Not eligible
- You are not required to participate in MIPS but may have an option to opt-in to report. Your ability to opt-in depends upon how much you billed Medicare.
- MIPS Eligible Clinician Individual
- As an individual clinician you are required to report.
- MIPS Eligible Clinician Group
- As an eligible clinician, you are part of a group that is required to report. Groups are made up of clinicians who all bill with the same Tax ID (TIN).
Once you identify whether you are eligible to report as an individual or group, you may choose how to participate.
- Individual: Collect and submit your data as an individual.
- Group: Collect and submit data for all clinicians in the group.
- Subgroup: (MVP only) Collect and submit data for all clinicians in the subgroup.
- Virtual Group: (MIPS only) Collect and submit data for all clinicians in a CMS-approved virtual group. Virtual groups must be established before the start of the performance year.
- APM Entity: Collect and submit data for the clinicians identified as participating in the MIPS APM.
APM Entities will be referenced throughout.
APM stands for Alternative Payment Model. An APM Entity is responsible for reporting to this program on behalf of their participants.
Advanced APM Entity
An organization that takes on some form of financial risk. These organizations do not have to report to MIPS.
Other APM Entity
Those organizations not designated as advanced. ACOs make up a good portion of these types of organizations.
Reporting Frameworks
Understanding the Frameworks
Once you know your participation status, you will understand which framework you can use for submission. There are three QPP frameworks in 2024:
Traditional MIPS Framework
This is the usual MIPS framework made up of four categories and a composite score.
APM Performance Pathway (APP) Framework
The APP Framework is available to MIPS APM Entities and required for ACOs if they are part of MSSP.
MVP Framework
The MVP framework focuses on sub-group reporting by specialty type – applicable specialty measures designed for specialists. This reporting framework will eventually replace Traditional MIPS.
Here is a matrix of which framework you can report to, based on your status.
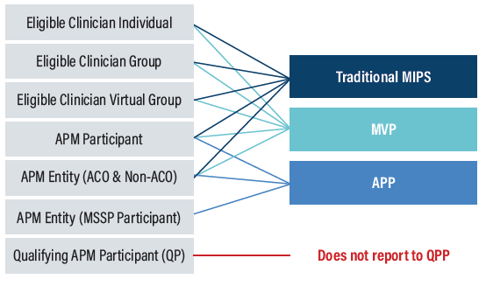
Each framework has slightly different requirements and different category weights.
Collection Types
Collection types are the way you report the data to CMS. You can think of them like measures. There are six collection types in 2024.
- eCQMs (Electronic Clinical Quality Measures)
- MIPS CQMs
- QCDR measures (Qualified Clinical Data Registry)
- Medicare Part B Claims measures
- CAHPS for MIPS survey
- CMS Web Interface measures (available for MSSP ACOs only)
As I mentioned before, CMS Web Interface is going away in 2025, so if this is the primary way you submitted your measures before, you need to figure out a new collection type soon.
Which collection type you can submit depends upon your participation status.
Now we are ready to review the requirements for each framework.
|
Learn how Medisolv helps hospitals navigate QPP changes in 2024 |
2024 Quality Requirements
Traditional MIPS Framework
Traditional MIPS Framework: Quality Category
Category weight: 30% of total MIPS score
Performance Period: 365 days
Requirements
- Submit 6 measures one of which is an outcome measure or high priority measure
- Report data for at least 75% of patients who qualify for a measure
- You may use a combo of collection types (listed below)
- Four administrative quality claims measures are calculated automatically
Measure List
- Quality Measures
- The 2024 measure list can be found here.
- Claims Measures
- Hospital-Wide, 30-Day, All-Cause Unplanned Readmission (HWR) Rate for MIPS Eligible Groups.
- Risk-standardized Complication Rate (RSCR) following Elective Primary Total Hip Arthroplasty (THA) and/or Total Knee Arthroplasty (TKA) for MIPS
- Clinician and Clinician Group Risk-standardized Hospital Admission Rates for Patients with Multiple Chronic Conditions
-
Risk-Standardized Acute Unplanned Cardiovascular-Related Admission Rates for Patients with Heart Failure for the Merit-based Incentive Payment System
Available Collection Types
- eCQMs
- MIPS CQMs
- QCDR measures
- Administrative claims quality measures*
- CAHPS for MIPS survey measures
- Medicare CQMs**
*Only small practices may submit quality measures using claims
**Available for MSSP ACOs
Other Considerations
Submitting the CAHPS for MIPS Survey will count as reporting one high priority measure. Select five other Quality measures to report, including an outcome measure if available.
There are no bonus points awarded for reporting additional outcome and high priority measures beyond the required one.
If you submit a new quality measure, there is 7-point minimum score awarded for submission in the measure’s first year and a 5-point minimum score awarded in its second year.
There is no floor for any measures submitted (with a benchmark). There used to be a minimum of 3-points, but that was removed in 2023.
Data Completeness Requirements
If a measure doesn’t meet the 75% data completeness threshold, the measure will earn 0 points in 2024.
Case Minimum
If a measure doesn’t meet case minimum requirements, the measure will earn 0 points in 2024.
APP Framework
APP Framework: Quality Category
Category weight: 50% of total score
Performance Period: 365 days
Requirements
Option 1
- Submit 3 eCQMs/CQMs or Medicare CQMs
- Meet data completeness requirements
- You may use a combo of collection types (eCQMs, CQMs, or Medicare CQMs)
- Two administrative quality claims measures are calculated automatically
- CAHPS for MIPS survey
Option 2
- Submit 10 CMS Web Interface Measures
- Report data for 100% of assigned Medicare beneficiaries identified by CMS (248 cases)
- Two administrative quality claims measures are calculated automatically
- CAHPS for MIPS survey
ACOs may do both.
Highest score will be assigned to the ACO when multiple scores are available.
Measure List
- Quality Measures (Option 1)
- eCQMs/CQMs
- Quality ID: 001 Diabetes: Hemoglobin A1c (HbA1c) Poor Control
- Quality ID: 134 Preventive Care and Screening
- Quality ID: 236 Controlling High Blood Pressure
- eCQMs/CQMs
- Quality Measures (Option 2)
- CMS Web Interface Measures
- Quality ID: 001 Diabetes: Hemoglobin A1c (HbA1c) Poor Control
- Quality ID: 134 Preventive Care and Screening
- Quality ID: 236 Controlling High Blood Pressure
- Quality ID: 318 Falls: Screening for Future Fall Risk
- Quality ID: 110 Preventive Care and Screening: Influenza Immunization
- Quality ID: 226 Preventive Care and Screening: Tobacco Use: Screening and Cessation Intervention
- Quality ID: 113 Colorectal Cancer Screening
- Quality ID: 112 Breast Cancer Screening
- Quality ID: 438 Statin Therapy for the Prevention and Treatment of Cardiovascular Disease
- Quality ID: 370 Depression Remission at Twelve Months
- CMS Web Interface Measures
- Claims Measures
- Hospital-Wide, 30-Day, All-Cause Unplanned Readmission (HWR) Rate for MIPS Eligible Groups.
- Clinician and Clinician Group Risk-standardized Hospital Admission Rates for Patients with Multiple Chronic Conditions
- CAHPS for MIPS Survey measure
Other Considerations
- CMS will still retire CMS Web Interface measures in 2025.
- To help ACOs who are struggling with the transition, CMS finalized a new collection type called Medicare CQMs.
- ACOs may now choose to submit eCQMs, CQMs, and/or Medicare CQMs.
- You may choose to submit different collection types for one submission.
Data Completeness Requirements
If an eCQM or CQM does not meet the 75% data completeness threshold, the measure will earn 0 points in 2024.
MVP Framework
MVP Framework: Quality Category
Category weight: 30% of total score
Performance Period: 365 days
Requirements
- Register for one or more of the 16 available MVPs between April 1-November 30, 2024
- Submit 4 quality measures within the specific MVP (for each MVP) one must be an outcome measure or high priority measure
- Report data for at least 75% of patients who qualify for a measure
- You may use a combo of collection types
Measure List
Each measure list is specific to the particular MVP. Download specific measure lists here.
Available Collection Types
- eCQMs (Electronic Clinical Quality Measures)
- MIPS CQMs
- QCDR measures (Qualified Clinical Data Registry)
- Administrative claims quality measures*
- CAHPS for MIPS survey measures
- Medicare CQMs**
*Only small practices may submit quality measures using claims
**Available for MSSP ACOs
Other Considerations
- There are no bonus points awarded for reporting additional outcome and high priority measures beyond the required one.
- If you submit a new quality measure, there is 7-point minimum score awarded for submission in the measure’s first year and a 5-point minimum score awarded in its second year.
- There is no floor for any measures submitted (with a benchmark). There used to be a minimum of 3-points.
Case Minimum
If a measure does not meet case minimum requirements, the measure will earn 0 points in 2024.
2024 Promoting Interoperability Requirements
Traditional MIPS Framework
Traditional MIPS Framework: PI Category
Category weight: 25% of total MIPS score
Performance Period: 180 days
Requirements
- Submit the required measures (measure list below)
- Attest to these two measures: Prevention of Information Blocking and ONC Direct Review
- Collect your data in EHR technology certified to the 2015 Edition or 2015 Cures Edition Update, or a combination of both
- Provide your EHR’s CMS Identification code from the Certified Health IT Product List (CHPL)
- Conduct or review a security risk analysis on your CEHRT functionality on an annual basis
- Attest to conducting an annual assessment of the Safety Assurance Factors for EHR Resilience Guides (SAFER Guides)
Measure List
Promoting Interoperability Measures
- e-Prescribing
- Query of Prescription Drug Monitoring Program (PDMP)
- Sending Health Information AND
- Receiving and Reconciling Health Information OR
- HIE Bi-Directional Exchange OR
- Enable Exchange Under TEFCA
- Provide Patients Electronic Access to Health Information
- Electronic Case Reporting
- Immunization Registry
- Public Health Registry
- Syndromic Surveillance
- Clinical Data Registry
Reweighting
Public Health and Clinical Data Exchange Objective has two Active Engagement options that must be completed for each associated measure:
- Option 1: Pre-production and Validation
- Option 2: Validated Data Production
Clinicians are required to report level of engagement for EACH measure and beginning in 2024 must transition from option 1 to option 2 after one year.
CMS is discontinuing automatic re-weighting for the following clinician types:
- Physical therapist
- Occupational therapist
- Qualified speech – language pathologist
- Clinical psychologist
- Registered dietitians or nutrition professionals
CMS will continue to automatically assign a weight of zero to this category for:
- Clinical social workers
CMS will continue to automatically reweight:
- Small practices
- Hospital-based and ambulatory surgical center-based clinicians
APM Entity
This year an APM Entity may submit Promoting Interoperability on behalf of the individual clinicians and groups they cover.
APP Framework
APP Framework: PI Category
Category weight: 30% of total score
Performance Period: 180 days
Requirements
Submit the required measures (measure list below)
- Attest to these two measures: Prevention of Information Blocking and ONC Direct Review
- Collect your data in EHR technology certified to the 2015 Edition or 2015 Cures Edition Update, or a combination of both
- Provide your EHR’s CMS Identification code from the Certified Health IT Product List (CHPL)
- Conduct or review a security risk analysis on your CEHRT functionality on an annual basis
- Attest to conducting an annual assessment of the Safety Assurance Factors for EHR Resilience Guides (SAFER Guides)
Measure List
Promoting Interoperability Measures
- E-Prescribing
- Query PDMP
- Sending Health Information AND
- Receiving and Recording Health Information OR
- HIE Bi-Directional Exchange OR
- Enable Exchange under TEFCA
- Provide Patients Electronic Access to Health Information
- Electronic Case Reporting
- Immunization Registry
- Public Health Registry
- Syndromic Surveillance
- Clinical Data Registry
Other Considerations
You must submit the PI Category:
- At an aggregate level on behalf of 100% of your Eligible Clinicians
OR - 100% of your Eligible Clinicians may submit as an individual or part of a group submission separately.
By 2025 ACOs must have all their practices off of paper and on Certified EHR Technology (CEHRT).
MVP Framework
MVP Framework: PI Category
Category weight: 25% of total score
Performance Period: 180 days
Requirements
Submit the required measures (measure list below)
- Attest to these two measures: Prevention of Information Blocking and ONC Direct Review
- Collect your data using an EHR technology certified by ONC to meet the 2015 Cures Update Certification
- Provide your EHR’s CMS Identification code from the Certified Health IT Product List (CHPL)
- Conduct or review a security risk analysis on your CEHRT functionality on an annual basis
- Attest to conducting an annual assessment of the Safety Assurance Factors for EHR Resilience Guides (SAFER Guides)
Measure List
Promoting Interoperability Measures
- e-Prescribing
- Query of Prescription Drug Monitoring Program (PDMP)
- Sending Health Information AND
- Receiving and Reconciling Health Information OR
- HIE Bi-Directional Exchange OR
- Enable Exchange Under TEFCA
- Provide Patients Electronic Access to Health Information
- Electronic Case Reporting
- Immunization Registry
- Public Health Registry
- Syndromic Surveillance
- Clinical Data Registry
Reweighting
Public Health and Clinical Data Exchange Objective has two Active Engagement options that must be completed for each associated measure:
- Option 1: Pre-production and Validation
- Option 2: Validated Data Production
Clinicians are required to report level of engagement for EACH measure and beginning in 2024 must transition from option 1 to option 2 after one year.
CMS is discontinuing automatic re-weighting for the following clinician types:
- Physical therapist
- Occupational therapist
- Qualified speech – language pathologist
- Clinical psychologist
- Registered dietitians or nutrition professionals
CMS will continue to automatically assign a weight of zero to this category for:
- Clinical social workers
Promoting Interoperability Measures
Query of Prescription Drug Monitoring Program (PDMP)
- Exclusion modified to the following: “Does not electronically prescribe any Schedule II opioids or Schedule III or IV drugs during the performance period”
Safety Assurance Factors for EHR Resilience (SAFER) Guides
- Requires a “yes” attestation response beginning with 2024
2024 Improvement Activities Requirements
Traditional MIPS Framework
Traditional MIPS Framework: IA Category
Category weight: 15% of total MIPS score
Performance Period: 90 days
Requirements
- Submit one of the following combinations of activities
- 2 high-weighted activities
- 1 high-weighted activity and 2 medium-weighted activities
- 4 medium-weighted activities
Measure List
Improvement Activity Measures
- The 2024 measure list can be found here.
Other Considerations
If you are submitting as a group at least 50% of your group’s clinicians must attest to completing the same improvement activity for 90 consecutive days. The activity may be completed anytime within the calendar year so long as each clinician attesting completes the activity for 90 consecutive days.
Patient-Centered Medical Homes
If you are a Patient-Centered Medical Home and more than 50% of your practices are recognized as a PCMH, you automatically receive full credit for this category.
APP Framework
APP Framework: IA Category
Category weight: 20% of total score
Requirements
All APM Entities reporting through the APP Framework will be automatically assigned a score of 100% which is applied to all Eligible Clinicians reporting through their APM Entity.
MVP Framework
MVP Framework: IA Category
Category weight: 15% of total score
Performance Period: 90 days
Requirements
- Submit one of the following combinations of activities
- 1 high-weighted activities
- 2 medium-weighted activities
Measure List
Improvement Activity Measures
- The 2024 measure list can be found here.
Patient-Centered Medical Homes
If you are a Patient-Centered Medical Home and more than 50% of your practices are recognized as a PCMH, you automatically receive full credit for this category.
2024 Cost Requirements
Traditional MIPS Program
Traditional MIPS Framework: Cost Category
Category weight: 30% of total MIPS score
Performance Period: 365 days
Requirements
- CMS will evaluate your performance on 29 claims measures.
Measure List
Cost Measures
- The 2024 measure list can be found here.
Other Considerations
If you don’t meet the established case minimum for any of the 29 measures to be scored, the cost performance category will receive zero weight when calculating your final score and the 30% will be distributed to another performance category (or categories).
APP Framework
Not applicable.
MVP Framework
MVP Framework: Cost Category
Category weight: 30% of total score
Performance Period: 365 days
Requirements
- CMS will evaluate your performance on cost measures via claims data.
- You will only be scored on the Cost measure relevant to your specific MVP.
Measure List
- Each measure list is specific to the particular MVP. Download your specific measure lists here.
2024 Population Health Requirements
Traditional MIPS Framework
Not applicable.
APP Framework
Not applicable.
MVP Framework
MVP Framework: Population Health Category
Category weight: Combined with your Quality Score
Performance Period: 365 days
Requirements
Select 1 of the 2 population health measures available at the time of MVP registration
- Q479: Hospital-Wide, 30-day, All-Cause Unplanned Readmission (HWR) Rate for the Merit-Based Incentive Payment System (MIPS) Groups
- Q484: Clinician and Clinician Group Risk-standardized Hospital Admission Rates for Patients with Multiple Chronic Conditions
Other Considerations
- CMS calculates performance based on administrative claims data.
- Score is calculated and included in the Quality performance category.
2024 Bonus Points
There are many opportunities to get bonus points within the MIPS program.
Improvement Bonus: Up To 10 Points
Clinicians will be rewarded if they demonstrate any improvement to their 2023 Quality score over the prior year (pending there is enough data for comparison). New Clinicians will be rewarded up to 1 additional point for improvement to their Cost performance scores.
Complex Patient Bonus: 5 Points
For clinicians who work with patients that have more complex cases, CMS will award up to 5 points to account for the additional complexity of treating their patient population.
Small Practice Bonus: 6 Points
An additional 6 bonus points will be added to the numerator of the Quality category for anyone qualifying as a small practice.
2024 Score Threshold Reimbursement
Applicable to MIPS and MVP Reporting Frameworks
To avoid a -9% penalty, you must score at least 75 points.
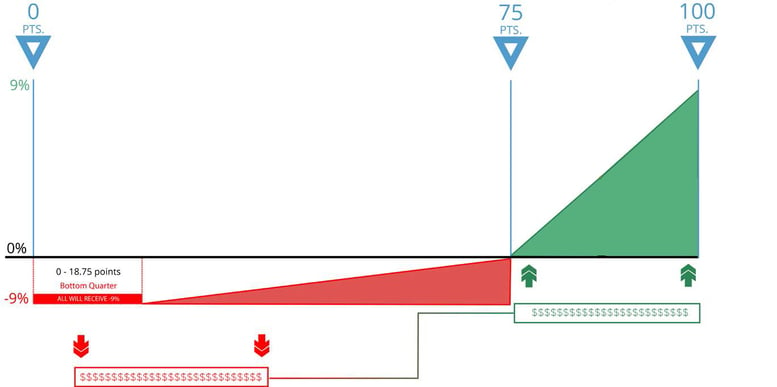
0-18.75 Points
If your score is between 0 and 18.75 points, you will lose -9% from your Medicare fee schedule (in red above).
18.76-74.99 Points
If your score is between 18.76 and 74.99 points, you will receive a reduction to your Medicare fee schedule between -8.99% and 0%
75 -100 Points
75 points is the performance threshold. CMS will take the funds of those who did not meet the threshold (in red) and distribute them among those who did meet the threshold (in green). Anyone whose MIPS score is between 75 and 100 points will receive some portion of those funds – up to a 9% increase to your Medicare fee schedule.
Note: There is no longer an Exceptional Performance bonus
APP Reporting Framework - MSSP ACOs
Shared Savings
To get the maximum shared savings for your ACO you must:
Report ALL measures in the APP measure set
AND
Achieve the Quality Performance Standard
CMS has implemented a sliding scale to give ACOs some percentage of the Shared Savings (not max) if they don’t meet the quality performance standards but do achieve a quality performance score equivalent to or higher than the 10th percentile of the performance benchmark on at least one of the four outcome measures.
Maximize Your Shared Savings
Quality Performance Standard
- Report eCQMs/CQMs
- Achieve a score = > 10th percentile on 1 outcome measure
- Achieve a score = > 40th percentile on at least 1 of the remaining measure
OR
Health Equity-Adjusted score of => 40th percentile across ALL quality performance scores
CMS will calculate 2024 and 2025 benchmarks for the Medicare CQMs based on performance period benchmarks. They will transition to historical benchmarks in 2026 and subsequent years.
This means that ACOs will not know the Medicare CQM benchmarks during the performance period.
CMS is NOT extending the eCQM/MIPS CQM reporting incentive to Medicare CQMs.
CMS finalized the use of historical data to establish the 40th percentile MIPS Quality performance category score used for the quality performance standard.
That means you would know what the Quality Performance Standard percentile is BEFORE the performance year starts.
40th Percentile MIPS Quality Performance Category Scores Used in the Calculation of the PY 2024 Historical MIPS Quality Performance Category Score
| Performance Year |
40th Percentile of the MIPS Quality Performance Category Score |
|
2020 |
75.59^ |
|
2021 |
77.83^ |
|
2022 |
77.73^ |
|
2023 |
Skipped due to 1-year lag |
|
2024 |
77.05 |
^ PY 2020 through PY 2022 40th percentile scores are based on performance period data
Important Dates
January 1, 2024
The start date to track 365 days of Quality and Cost category measures.
April 1, 2024
Registration opens for CMS Web Interface, CAHPS for MIPS Survey, and MVP selection.
July 4, 2024
The last day to start measures in the Promoting Interoperability category to meet the minimum of 180 continuous days.
October 2, 2024
The last day to start Improvement Activities to meet the minimum requirement of 90 continuous days.
November 30, 2024
Last day to register for an MVP.
March 31, 2025
The last day to submit all of your performance data.
Medisolv's QPP PackageMedisolv Can HelpThis is a big year for Quality. Medisolv can help you along the way. Along with award-winning software you receive a dedicated Medisolv Clinical Quality Advisor that helps you with all of your technical and clinical needs with no time restraints or extra costs.
|




.png?width=352&name=BlogImage_2025%20APP%20Reporting%20Requirements%20for%20ACOs%20(2).png)
Comments