eCQM vs CQM vs Web Interface: Understanding the Difference

In the Quality Payment Program, there are several different types of quality measures available for the Quality category. You may have heard various terms thrown around: eCQM, CQMs, QCDR measures and CMS Web Interface measures.
Depending upon your organization’s situation, one of these "collection types" (as CMS refers to them) may be better suited for your needs. Typically, most organizations find themselves debating on whether they should use eCQMs or CQMs to meet their Quality category data requirements.
This is particularly relevant to MSSP ACOs as they decide which measure type they will move forward with when CMS officially retires the CMS Web Interface measures in 2025.
So, what's the difference between those measure types?
Today, we are going to review the difference between these three common measure types.
Web Interface Measures
We are going to start with the Web Interface measures because it is quite different than the other two options.
Web Interface measures are basically a sampling of patients from which you enter the data for each patient.
This is the primary way that ACOs have been reporting quality measure performance in the Quality Payment Program. In fact, at the 2022 Fall NAACOs Conference this week CMS reported that only 12 (12!) ACOs out of more than 500 ACOs submitted eCQMs. Five reported using CQMs and the rest all used Web Interface measures. By 2025, all MSSP ACOs will need to report either eCQMs or CQMs.
With Web Interface measures, CMS provides an organization a list of patients for each of the 10 required measures. The reporting organization selects a list of 248 patients (Medicare only) to report their results.
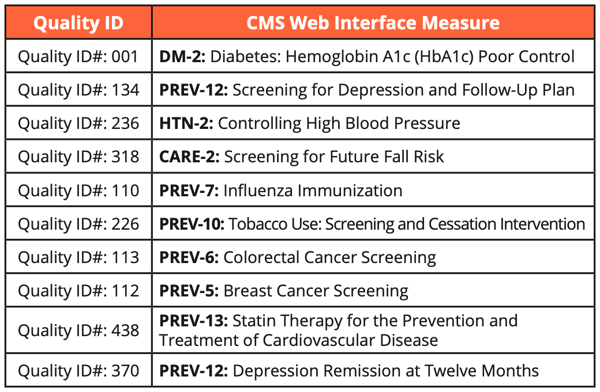
Here’s the list of measures included with Web Interface.
Now let’s move to the differences between eCQMs vs CQMs.
One important thing to note here applies to these two measure types versus the Web Interface measures. Unlike Web Interface which is Medicare patients only, both CQMs and eCQM require you to report for all patients, all payers across all practices. Wow. Let that sink in for a minute. The “all payers” requirement has huge ramifications if you’re an ACO organization. Don’t underestimate what it will take to make a transition away from CMS Web Interface measures to one of these two other measure types.
The Difference Between Capturing eCQMs vs CQMs
The main difference between eCQMs and CQMs is that eCQMs require structured data to be captured electronically, often at the point of care, while in most cases, CQMs have some level of additional manual data collection from the medical record often referred to as data abstraction.
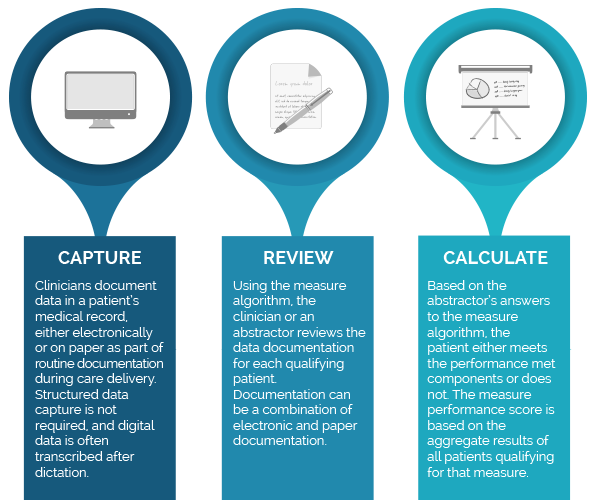
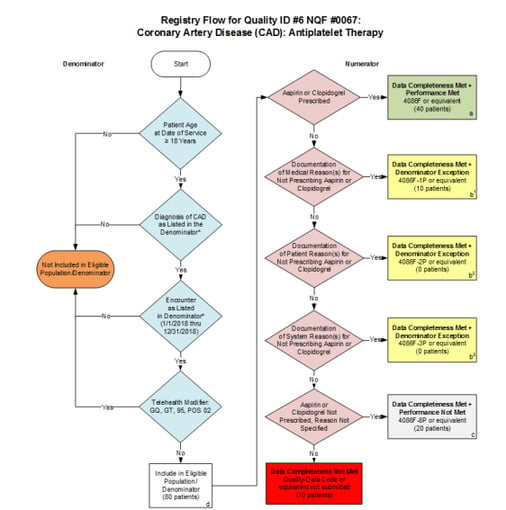
For example, with MIPS CQMs, an abstractor can review the patient’s records (electronic and paper documentation) to assess whether the patient has passed or failed the measure. Even if a physician documented in a hand-written note that they prescribed aspirin for the patient, an abstractor could use that documentation to confirm that the patient did pass the CQM #0067: Coronary Artery Disease (CAD): Antiplatelet Therapy.
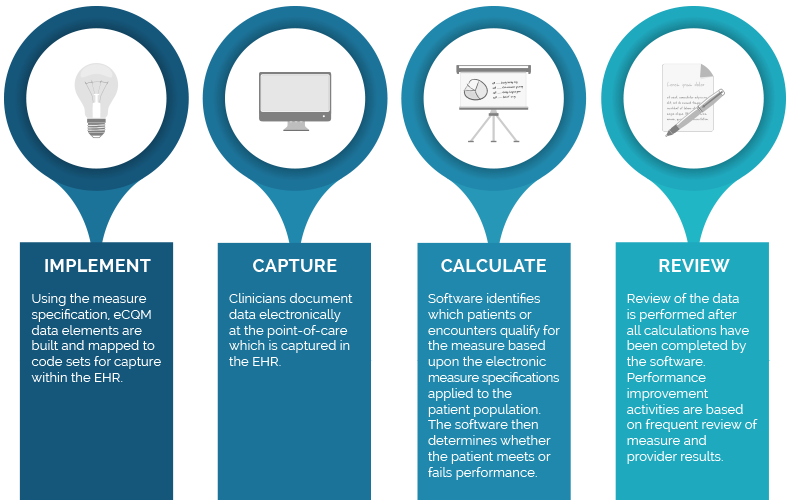
With eCQMs, the clinician documents in a structured field within the Electronic Health Record (EHR), usually as part of a clinical workflow ( e.g., ordering a medication using an electronic order entry system or documents a valid reason for not doing an expected intervention). This data is consumed by the eCQM calculation engine without additional manual data entry.
Below we summarize differences in both types of measures.
eCQM Process
CQM Process
The Difference in Calculating eCQMs vs CQMs
In addition to differences in data capture, the specifications and result calculations are also quite different.
Comparing Specifications
The specifications for each measure differ significantly as well. Let’s take a look at the differences between the specifications at a very high-level.
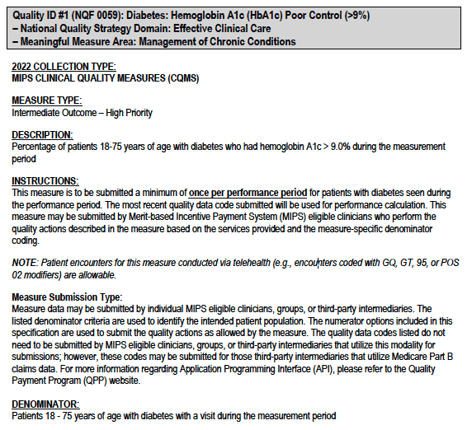
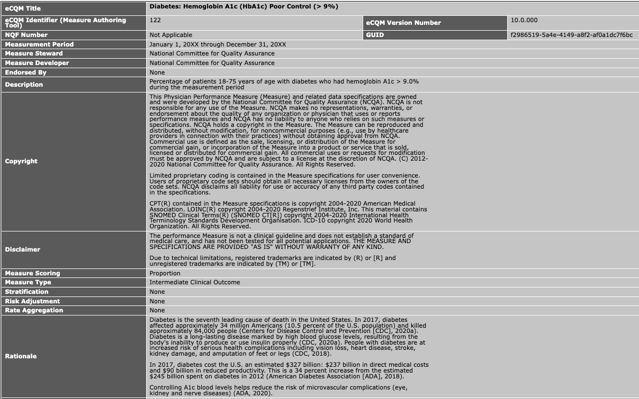
If you compare the descriptions, it all looks pretty similar. Each measure has a name, type, description and rationale.
|
CQM Description Section |
eCQM Description Section |
| DM-2: Diabetes Hemoglobin A1c (HbA1c) Poor Control |
CMS122: Diabetes: Hemoglobin A1c (HbA1c) Poor Control |
|
|
Now let’s review the logic.
|
CQM Specification Logic (Algorithm) |
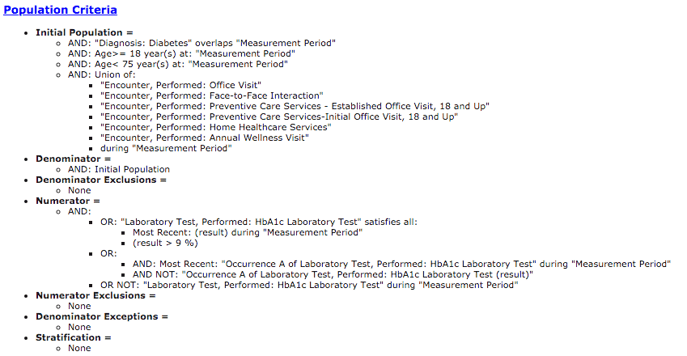
eCQM Specification Logic |
| DM-2: Diabetes Hemoglobin A1c (HbA1c) Poor Control |
CMS122: Diabetes: Hemoglobin A1c (HbA1c) Poor Control |
 |
 |
When you get to the logic, it starts to look different. With the CQM, a nice visual guides the abstractor through the measure. As you answer yes or no, it will lead you to the correct end result.
In the eCQM logic, you will see a bunch of computer logic, which guides a computer through the measure logic and places patients into the appropriate population (e.g., Numerator, Denominator, Exclusion, etc). Data elements in the EHR are mapped to codes. Each line you see in that logic will require a corresponding code to ensure that it’s captured correctly. If there isn’t a code present or if it’s the wrong code or if the documentation is not in the EHR, the patient may fall out of the measure.
Why would an organization choose eCQMs vs CQMs?
This decision often comes down to two things – time and money. What’s the balance between how much it would cost to aggregate all of the data streams required for eCQM calculation versus the amount of time and resources it would take to abstract every single patient encounter.
One other thing to consider is the CMS shift to Digital Quality Measures. CMS very clearly stated in their dQM Strategy Roadmap that they intend to push the industry to universal adoption of digital quality measurement – as opposed to allowing manual intervention.
As you consider your options for reporting eCQMs vs CQMs consider the long-term strategy for your organization.
Maybe it’s not about choosing one over the other
CMS recognizes that for those organizations (not ACOs) that are submitting traditional MIPS and are facing transitioning to the MIPS Value Pathways (MVP) reporting option there aren’t as many eCQMs that are applicable to the specific MVP specialty type. If and when you transition to MVP reporting (at a sub-TIN level) you may find yourself doing a combination of CQMs and eCQMs and maybe even QCDR measures in order to meet your Quality requirement.
It might not be as straightforward as picking one measure type and sticking with it. CMS is trying to provide flexibility in measure types so that an organization can find the measures that work for their specialty group. The bottom line is that CMS wants the data.
Retiring the Web Interface Measures
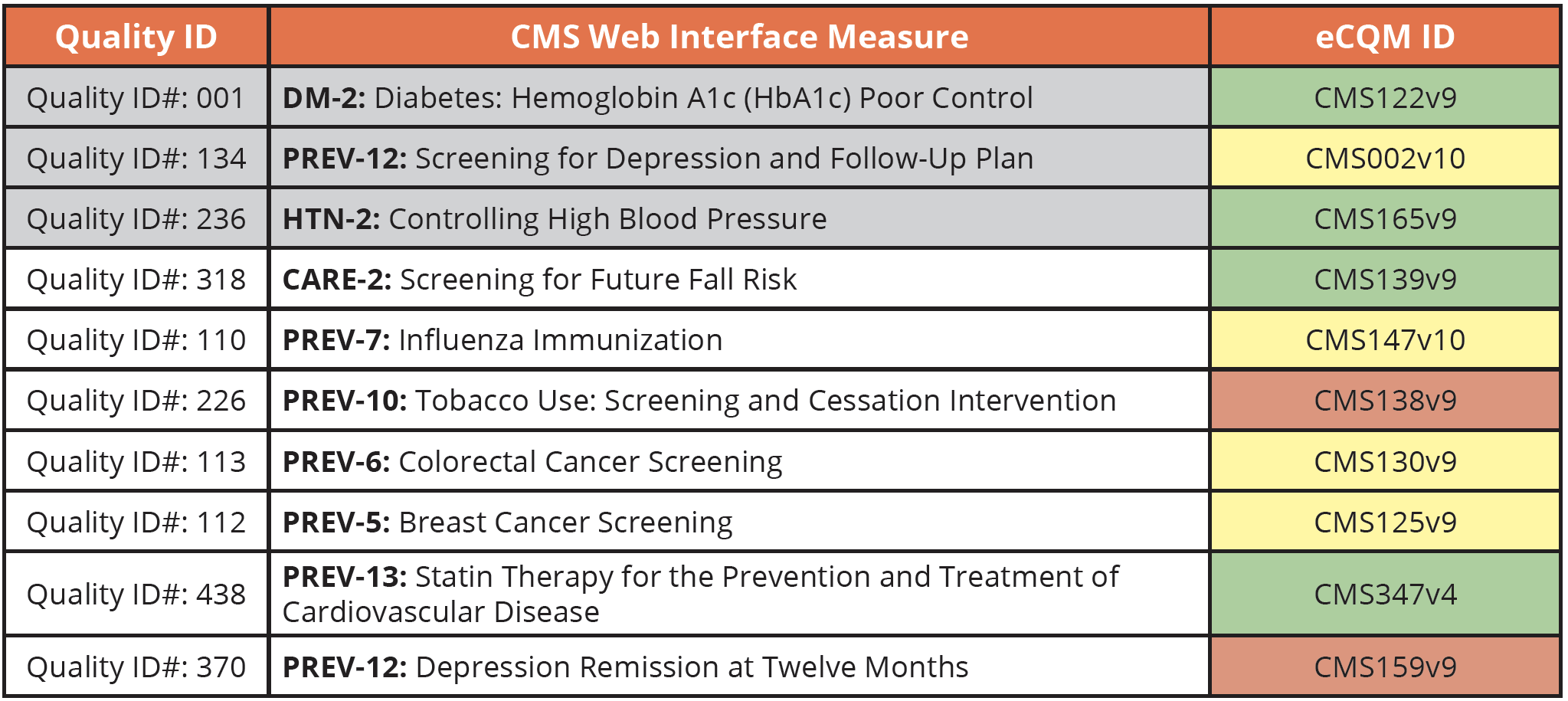
As a reminder, the CMS Web Interface measures will be sunset by 2025. If you previously submitted these measures, you must now choose a different measure type. Instead of the 10 Web Interface measures you’ve submitted up until now, those reporting using the APP framework must submit three eCQMs or CQMs (highlighted in gray in the chart below). Remember this is for all payers, all patients across all your practices.
For additional help, download our Guide to Transitioning from the CMS Web Interface measures.
Here is a cross walk from the guidebook to help you find equivalent eCQMs. This is just our opinion here, but as we’ve worked with clients to implement these measures over the years, we’ve found some to be easier than others. Green is easy, yellow is a bit difficult, and red is very difficult.
I hope this quick summary of the differences between eCQMs vs CQMs vs Web Interface measures was helpful. If you need help submitting your Quality data using eCQMs and CQMs, schedule a 1 on 1 call with us. We’d love to hear about your situation and see if we can assist.
Medisolv can helpAlong with award-winning software, each client receives a dedicated Clinical Quality Advisor that helps you with your technical and clinical needs. We consistently hear from our clients that the biggest differentiator between Medisolv and other vendors is the level of one-of-one support. Especially if you use an EHR vendor right now, you’ll notice a huge difference.
Here are some resources to help you get started:
|

.png?width=352&name=2026%20Quality%20Reporting%20Deadlines%20Guide%20(1).png)



Comments