The Changing World of Quality in 2017

Happy New Year! The year 2017 will bring about exciting changes for those working in the health care space. In this week’s blog, our CEO, Dr. Zahid Butt, sat down to write about the current state of quality in the hospital setting and how he sees quality changing in the coming year. From all of us here at Medisolv, we wish you and yours a blessed and prosperous new year. Enjoy!
We are witnessing profound changes in the health care space right now. Every aspect of the health care enterprise is in play,including revenue, costs and market share to name a few. We are confronting alternative payment models, such as bundled payments and shared savings programs. Fee-for-service payments are being linked to Quality through Value-Based Payment Models. Consumerism in health care is being encouraged through both public reporting and also through provider accountability for the health of their populations even though the definition of population health is still a work in progress. Quality is central to every one of these shifts in health care. Therefore it should be no surprise that everything we do in Quality is also changing quite rapidly.
Quality up until now
Until recently, Quality was mostly limited to reporting a fair number of process numbers, usually in the hospital setting, typically organized as measure sets around specific diseases or procedures. Each inpatient record was painstakingly reviewed after discharge to abstract the data. Submission of these data by certain deadlines usually meant that you had met the reporting requirement. Other than some public reporting on Hospital Compare, there was not much incentive, certainly not payment incentives for better performance.
Data quality was generally good due to internal reviews supplemented with random audits by CMS. The rules around abstraction drove many of the clinical documentation or CDI initiatives. Clinicians were asked to simply document relevant facts in whatever fashion they could, including writing by hand. As long as a human abstractor could find something, it was usually good enough.
Quality today
Quality has changed quite a bit now. For one thing, the number of process measures has reduced dramatically with a corresponding increase in the number of outcome measures. The newest in that category being reported by patients themselves is known by the acronym PROMs (Patient Reported Outcomes Measures). While both payers and patients are more interested in outcomes compared to process of care measures, it doesn’t mean that process of care measures are not important. Perhaps in the future, good process measures will be used internally to improve the outcomes rather than for external reporting.
The remaining process measures are being replaced by Electronic Clinical Quality Measures also known as eCQMs. These made their first appearance in the Meaningful Use program and are now making their way into the true quality reporting programs with submission of electronic data files formatted in the QRDA I standard.
Another big adjustment is the change to pay-for-performance, which is replacing pay-for-reporting. Finally performance is hitting its stride and will matter more than ever. The data quality of eCQMs is still being evaluated. Medisolv has done some work for CMS in this area by comparing eCQMs to their abstracted counter-parts, which is one way to ensure eCQM data quality. CMS performed a voluntary validation pilot in 2014 and CDAC audits are scheduled for 2018.
CMS’ vision for electronic quality measures
CMS is clearly leading the charge for electronic quality initiatives and it is no surprise since they have been heavily involved in quality reporting for quite some time. The chart below outlines the major CMS quality reporting programs.
CMS Quality Reporting Programs

Using the various documents CMS has released – through in-person presentations, webinars, final rules and other materials – I will highlight the trends I see emerging in 2017 and beyond.
The switch From Traditional Fee-for-Service
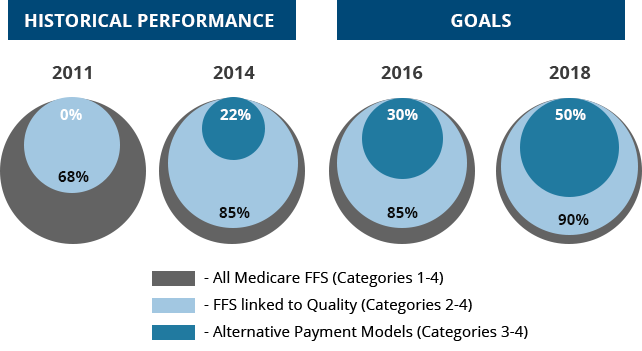
CMS has made it very clear that they intend to increase the fee-for-service payments linked to Quality and move to Alternative Payment Models. In fact, CMS’ stated goal is to have 50% of their payments to be linked to Alternative Payment Models by 2018 and 90 percent of fee-for-service payment directly linked to Quality in the same time frame. This is part of their strategy to shift from volume to value, which at its core, is modeled after the Triple Aim.
Historical Performance vs. Goals of the Payment Models
The Triple Aim
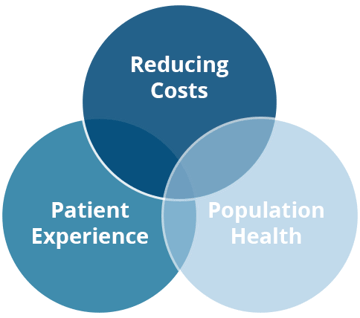
I’m sure most of you are familiar with the Triple Aim as championed by Dr. Donald Berwick. The Triple Aim links Quality and Cost to a Population Health framework. The context is that of a payer such as a health plan or even a risk-baring provider entity and the population refers to a defined group of covered lives attributed to the entity.
Report once strategy
Another vision articulated by CMS is due, in part, to provider complaints regarding excessive reporting burden. CMS aims to consolidate their programs in a way that providers have to report only once and get credit for multiple programs aligned along certain priorities. Thus was born the National Quality Strategy through the convened National Quality Forum Stakeholder Groups.
National Quality Forum Stakeholder Groups

Components of this are shown on the right column. The column on the left shows the CMS measure domains which map directly to the National Quality Strategy. You may have already noticed that many quality measures for both hospitals and providers are categorized in these domains instead of the usual disease and procedure measure sets.
Program Alignment
By far the most significant CMS Quality Reporting Program alignment however is between Meaningful Use and the CMS quality reporting programs for both Eligible Hospitals (EHs) and Eligible Providers (EPs). Starting next year, Meaningful Use for EPs will be absorbed into the MACRA legislation, which is known as the Quality Payment Program (QPP). On the hospital side, Meaningful Use quality reporting is being aligned with the Hospital Inpatient Quality Reporting (IQR) program so that a single submission of electronic QRDA I files will give credit for both IQR and Meaningful Use.
eCQM data on the hospital side will not be used for public reporting or value-based purchasing for another couple of years. While there will be a consolidation between the programs for providers and hospitals, they still have multiple types of measures to deal with, particularly in the hospital IQR program, such as electronic, chart-abstracted and claims-based measures.
Quality Reporting Requirements
Let’s review the external reporting requirements that are in play for Eligible Hospitals and Eligible Physicians in the upcoming year.
The Joint Commission
The ORYX accreditation reporting requires five chart-abstracted measures for hospitals with less than 300 live births per year, and an additional four abstracted measures for those with greater than 300 deliveries. Six out of 13 eCQMs are required to be reported as QRDA I files for all four quarters of 2017. As of our last information from The Joint Commission, they will be opening the submission portal in October of 2017. This means that even though there are quarterly submissions, the submissions will start sometime later in the year. The abstracted measures need to follow their usual quarterly submission deadlines.
Read more about The Joint Commissions’ requirements for 2017.
CMS IQR Program
CMS, on the other hand, has six required chart-abstracted measures, five are similar to The Joint Commission, and additionally the sepsis bundle measure. Six NHSN measures have to be reported; five of which are hospital acquired infections and one healthcare professional influenza vaccination measure. There are nine HCAHPS measures and two structural measures including the patient safety culture survey and safe surgery checklist. Next year, the number of required eCQMs doubles to eight. Hospitals must choose eight out of 15 eCQMs to report for the entirety of 2017. Read more about the CMS IQR program requirements for 2017.
2017 eCQMs (15) in which to choose from for required reporting
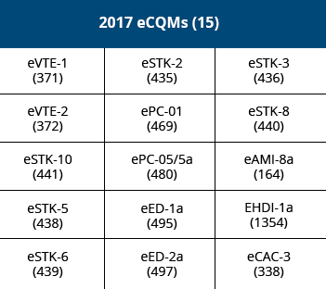
All these measures except eCQMs are reported on Hospital Compare with eCQMs not used for Value-Based Purchasing calculations.
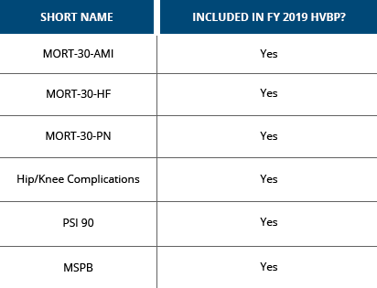
A quick note on claims-based measures
Claims-based measures tend to fly under the radar of some Quality professionals because they are not directly involved in submitting this data since CMS uses billing data to calculate these measures. Some of these measures are methodologically difficult to replicate outside CMS. For example, data for 30-day post-discharge mortality is difficult to get. And in the 30-day readmissions, patients who get admitted to hospitals outside the system are sometimes hard to track. However, one can still use the in-hospital mortality rate and readmissions to hospitals within the system as a reasonable proxy compared to not having anything on an ongoing basis to understand your performance. I’ve highlighted the measures that are also used for the Value-Based Purchasing calculation.
CMS 2017 Claims-based Measures
Another claims-based measure that is very important in the Value-Based Purchasing calculation is the PSI 90 measure. This is a composite measures comprised of eight individual measures which was developed by AHRQ as a part of its patient safety indicator measure set. In PSI 90, as is true in most other composite measures, you need to decompose the measure into individual measures in order to address each one if you are going to improve the performance of the composite measure itself.
CMS Quality Payment Program (MACRA)
I am sure everyone has heard about MACRA by now. CMS prefers the acronym QPP (Quality Payment Program). This program consolidates three separate CMS programs, including Meaningful Use, Physician Quality Reporting System (PQRS) and the Value-Based Modifier program.
The QPP consists of two arms, the Merit-Based Incentive Payment System (MIPS) and the Advanced Alternative Payment Model (AAPM). In 2017, the MIPS arm is estimated to apply to 85% of providers. The AAPM arm will apply to roughly 15% of providers. CMS is trying to gently ease providers into this new system. Providers can pick their pace in reporting for MIPS with five options.
QPP Reporting Options
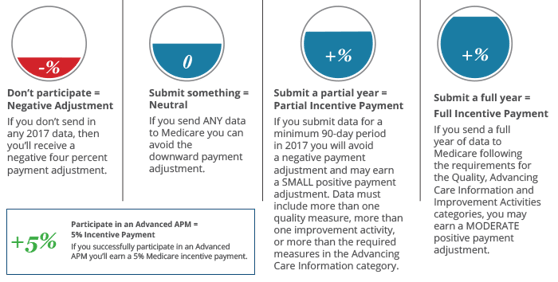
Option #1
Don't submit anything. Option #2
Submit something.
Option #3
Submit a partial year.
Option #4
Submit a full year.
Option #5
Participate in an AAPM.
Option two is the bare minimum, reporting just one measure will allow providers to avoid the penalty, while option four could yield quite a bit of upside payment adjustment. Those practices that are ready for MIPS should choose option four as it has the best potential for a maximum upside payment adjustment. If you qualify for option five, the AAPM, you can opt out of MIPS altogether and receive a 5% bonus payment. Please note that data submitted for calendar year 2017 will be used for payment adjustments in 2019. Any opportunity to improve needs to be addressed early in 2017.
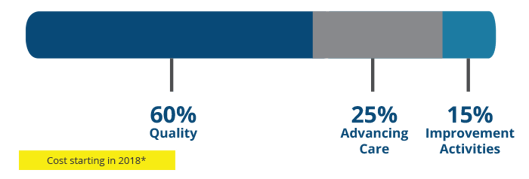
MIPS Categories
If your physicians take the MIPS path, they will be assessed based on their performance with the four MIPS categories; Quality, Advancing Care Information, Improvement Activities and Cost.
MIPS Categories Assessment
Quality Category
The Quality category replaces the PQRS requirement. It has a 60 percent weight. There are a total of 271 measures to choose from. They are categorized according to specialty sets and run the whole gamut of claims measures, group-practice reporting, web interface registries and EHRs. There are 53 available eCQMs from the ambulatory practice set. Reporting can be done as individuals or groups.
Advancing Care Information Category
The Advancing Care Information category replaces the Meaningful Use objective measures. There are five required measures in this category. Most of these are fairly simple. Submission of additional measures – up to nine – can be reported to get an additional bonuses.
Improvement Activities Category
A new category called the Improvement Activities category has also been added which comes with a choice. Providers can attest to having completed four out of 93 improvement activities. An alternative approach is for primary physicians to be a Patient Center Medical Home or for the specialist to be Patient Center Specialty Practice. As long as it is recognized by a certified program, such as NCQA or The Joint Commission, it can be used to get full credit for this category without having to do the individual activities.
Cost Category
The Cost category replaces the Value-Based Modifier program and is calculated by CMS using claims data so no data submission is required. It is currently set at 0% weight for 2017, but over the next three years, it will rise to 30%.
Understanding eCQMs
Let’s switch gears now and focus a bit on the eCQMs, starting with a basic definition. The NQF definition of an eCQM is “a standardized performance measure specified in the accepted standard Health Quality Measure Format (HQMF) that uses the Quality Data Model (QDM) and value sets vetted through the National Library of Medicine’s Value Set Authority Center (VSAC). Alternate forms of EHR specifications other than HQMF are not considered eMeasures. “
The important thing to note is that these measures are a completely different way of doing quality measurement. They are a standard space, fully-automated system from data capture to data submission without any human intervention. That places a big burden on hospitals to implement these and deal with eCQMs.
The life of an eCQM
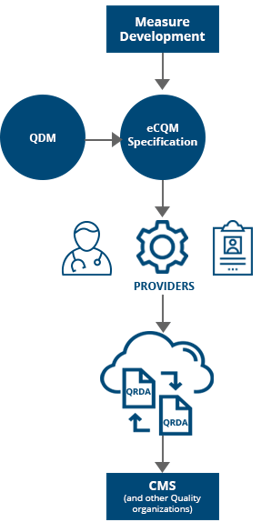
The lifecycle of an eCQM starts with measure development, which includes the creation of specifications in HQMF using something called the measure authoring tool. It uses the Quality Data Model as the underlying model for data elements and creates both human readable and machine readable formats conforming to the HQMF standard.
After the measure is developed and approved, it is implemented in the hospital setting. Hospitals must map the data elements to the qualifying codes from the associated value sets. Clinicians then capture the required structured data during their routine documentation while caring for patients. This documentation is evaluated for eCQM qualification.
Patient data and eCQM specifications are then consumed using an eCQM engine to create measure results. The output of this is in the Quality Reporting Data Architecture (QRDA) format which can either be at the patient level as QRDA I files or at the aggregate level as QRDA III files.
I think it is fair to say that it hasn’t been very easy for most hospitals to implement eCQMs because of the many moving parts shown here. Understanding the specifications and incorporating the annual updates in the eCQM software and EHR clinical workflows requires coordination between multiple entities and individuals. Accessing data from multiple sources and finally performing data validation presents unique challenges. The good news, however, is that even though it appears overwhelming at first, it is indeed quite doable and once you have done all of the hard work upfront, the underlying submission is a relatively simple process. Very different from the hustles around submission deadlines in the abstraction world.
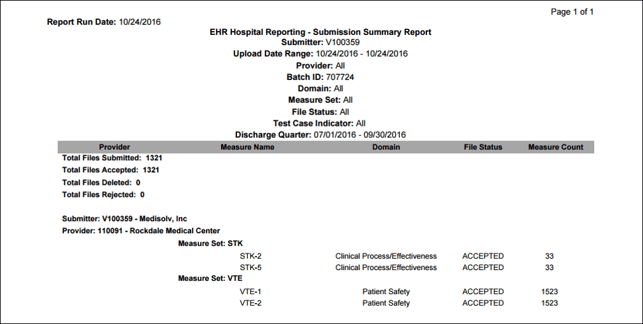
Once eCQMs are submitted to the CMS IQR program, hospitals receive an acknowledgement of successful eCQM submission (below). Medisolv has successfully submitted over 140,000 patient files on behalf of our clients in a relatively short period of time without any major issues. All of this to say that there are benefits to preparing well and completing data validation because then when it comes time to submit, you are ready.
Acknowledgement of Successful eCQM Submission Example
eCQM & Clinical Decisions Support Standards Alignment
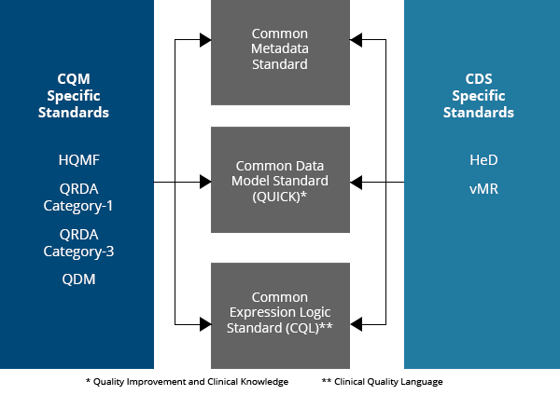
eCQMs and Clinical Decision Support (CDS) are two sides of the same coin. They have thus far operated quite independently. At least from the standards standpoint. Below is a comparison of the current state and the future vision of eCQMs and CDS as indicated by HealthIT.
Current State vs. Future Vision of eCQMs and CDS
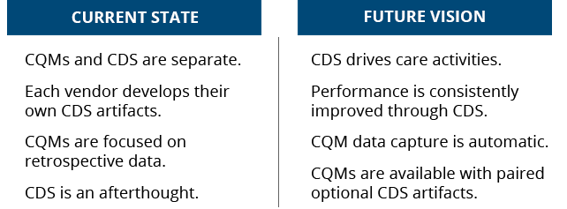
On the left-hand side, the current state shows that eCQMs and CDS are separate endeavors. Each vendor develops their own CDS artifacts and there is no collaboration between the two in most instances. The future vision is where CDS drives care activities while the eCQM data is captured automatically in a more near-real time basis. Ultimately the goal is for eCQMs and CDS artifacts to be paired and shared.
And to that end, ONC is leading an effort to harmonize the eCQM standards with those of the CDS. The quality measure standards are shown in dark blue on the left and the CDS standards are shown in light blue on the right. There is a harmonization effort and the goal is to ultimately have a shared interoperability common standard that would support both eCQMs and CDS.
CQM vs. CDS Specific Standards
The Future Role of the Quality Professional
So far we have covered many of the cross currents that are sure to impact the lives of Quality professionals. Let’s now focus on the Quality professional’s role in contributing to the culture and collaboration necessary for a technologically-advanced, high-performing organization.
Alignment starts at the top with the executive and board leadership and filters down to the key departments and individual clinicians. Everyone needs to understand the mission and goals. Otherwise, as they say, culture will eat strategy for lunch most days. In addition to excellent communication skills, Quality professionals will also need to have a working knowledge of data standards to effectively interact with the IT departments and software vendors as needed. Given the impact of Quality on payments, finance should also be included on the list of departments that may be involved in the future with the Quality professionals, if they aren’t already.
With the dramatic rise in acquisition of physician practices by hospitals and health systems, Quality professionals, will most likely be called upon to also support quality reporting in these practices. Engaging with physicians around quality improvement across multiple settings of care and team-based care is becoming increasingly important.
In order to fully support the physicians’ needs, the Quality professionals will also require a good understanding of what’s happening in the physicians’ world. Understanding the Quality Payment Program will be crucial. You can catch up on the basics with our eBook, the Basics of MACRA here.
And finally, I want to bring to your attention what is happening on the public reporting front. Hospital Compare has been around for some time and Physician Compare has been around for a few years. However, the uptake by the consumer has not been great. In order to make these websites more user friendly and useful for consumers, CMS has implemented the star system. The star system is based on these domains; mortality, safety of care, readmissions, patient experience, effectiveness of care, timeliness of care and efficient use of medical imaging.
CMS' Star System Ratings
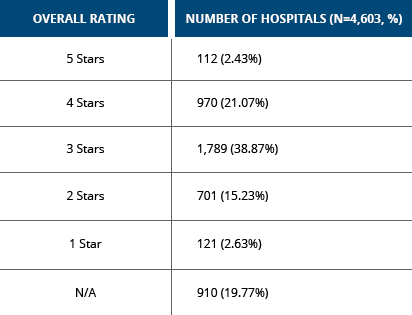
Only 2.43% of hospitals received five stars and 15% of hospitals received two stars. There is concern expressed by some institutions, as well as some organizations, that perhaps CMS could improve upon the methodology of the star ranking system. While there were calls to even get rid of the star ranking system, CMS has resisted that so far. I’m confident that there will be improvements in this as we go forward, but the point is that there is an aggressive attempt to use performance data for consumers to make choices about their healthcare and the selection of healthcare providers.
How and Why
So how should one approach this complexity? As I mentioned already, performance improvement is a key objective going forward. In order for you to improve performance there must be a solid measurement foundation and a culture of quality and safety that not only provides strong leadership support, but also uses measurement data to drive improvement interventions. Measurement for the sake of measuring will not by itself lead to improvement. A strong Health IT, analytics-enabled infrastructure is highly desirable. Simply saying that, “We are doing it” is not going to be enough. Unless it’s reported, it is not considered done.
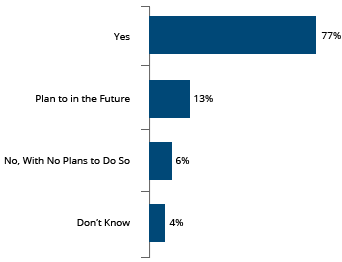
The question always arises, “What is the benefit of doing all of this?” I point to this recent HIMSS survey that suggests that the majority of health systems feel that EHRs on balance improve clinical quality performance. And so I believe that it is important to continue down this path not just for quality reporting but also for quality improvement. That is indeed where the federal government is focusing its attention. Now that 98% of hospitals have implemented EHRs, ONC and other stakeholders are beginning to focus on using these systems for performance improvement.
Impact of EHR on Clinical Quality Performance
In summary, while the changes I have mentioned may be too rapid and too fast for some and perhaps unsettling for many, they also offer tremendous opportunity for Quality professionals. It will, however, require the Quality professionals to develop their leadership skills, own the Quality domain and collaborate and coordinate with multiple stakeholders. It will also require education and knowledge around the changing world of Quality measures and the coordinating reporting program requirements. Quality professionals will need to develop a range of new skills including electronic quality measure implementation and validation. Equipped with these new skills, knowledge and initiative, Quality professionals can become the leaders in their organization.






Comments