CMS Web Interface: Options for Transitioning to a New Reporting Method
The Quality Payment Program (QPP) has allowed large organizations to use the CMS Web Interface reporting method to complete MIPS requirements since the program launched in 2017. This gave these organizations the option to report a sampling of 248 patients (selected by Medicare Part B claims) across all of their practices. CMS will completely sunset the CMS Web Interface reporting option by 2025, but begin phasing it out in 2023. In 2023 and 2024 only MSSP ACOs may continue to use the CMS Web Interface measures.
In 2025, all MSSP ACOs must report either eCQMs or CQMs for all patients, all payers, all practices for 365 days of the year.
Figuring out data aggregation, de-duplication and comprehensive performance review before 2025 is key to your success.
In this article we will review your CMS Web Interface options and then show you equivalent measures to help you make the digital measurement transition.
This post focuses exclusively on the Quality category requirements for the Quality Payment Program. For a full list of all requirements, please download our 2022 MIPS eBook.
Reporting Frameworks
If you currently report using the CMS Web Interface measures you can still do so through 2024. That being said, you must understand the new reporting framework options.
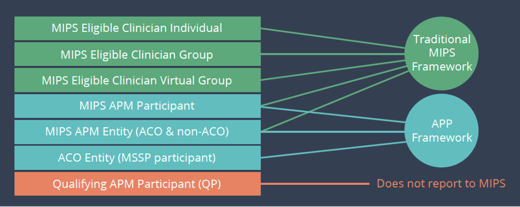
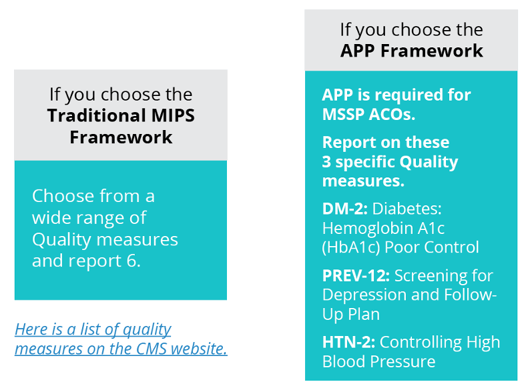
There are two MIPS frameworks. Each framework has slightly different requirements and different category weights.
Traditional MIPS
and
APM Performance Pathway (APP)
Traditional MIPS Framework
This is the usual MIPS framework made up of four categories and a composite score.
APM Performance Pathway (APP) Framework
The APP Framework is new and is available to MIPS APM entities and required for ACOs if they are part of MSSP.
Here is a matrix of which framework you can report to based on your status.
Requirements and Options for CMS Web Interface
We assume you know most of the information below but just in case, these are the requirements and measures for submitting the Quality category data to CMS using the CMS Web Interface collection type.
Note: There is a slight change in the Claims measure list and this is dependent upon which reporting framework you use.
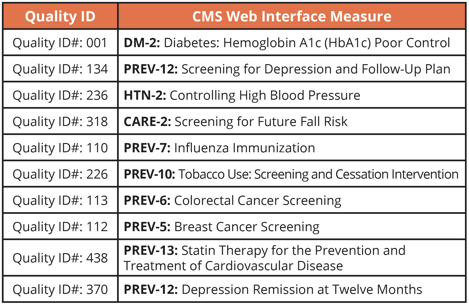
Quality Category: CMS Web Interface Collection Type
Requirements:
Must be a group, virtual group or APM entity with 25 or more eligible clinicians
- Submit all 10 measures listed below
- CMS generates and sends your organization samples of cases for each measure from Medicare part B claims
- You must submit 248 consecutive cases per measure from that sample
- Two administrative quality claims measures are calculated automatically
- CAHPS for MIPS survey
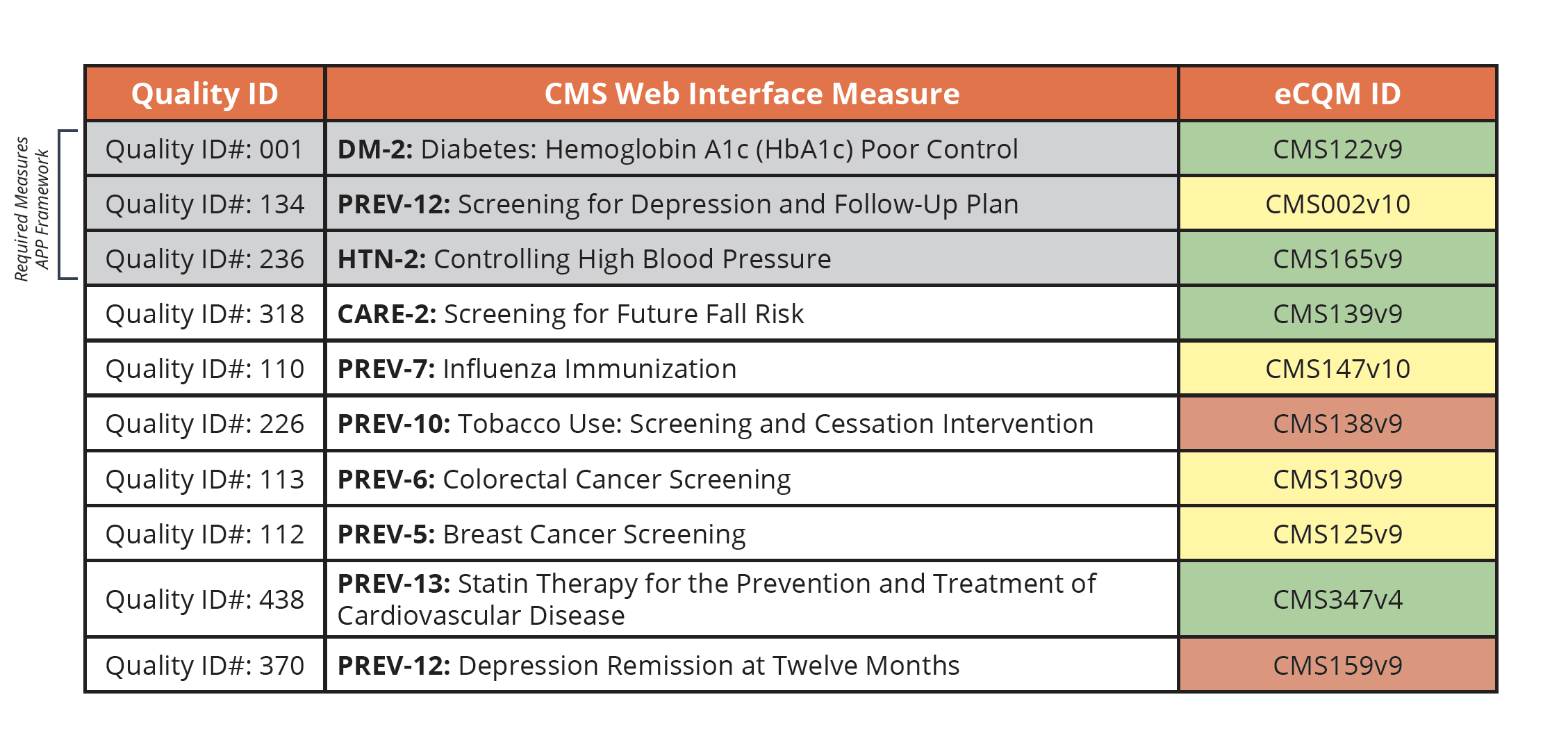
Measure List: Quality Measures
Measure List: Claims Measures
- Traditional MIPS Framework
- Hospital-Wide, 30-Day, All-Cause Unplanned Readmission (HWR) Rate for MIPS Eligible Groups. This measure is replacing the All-Cause Hospital Readmission (ACR) measure
- Risk-standardized Complication Rate (RSCR) following Elective Primary Total Hip Arthroplasty (THA) and/or Total Knee Arthroplasty (TKA) for MIPS
- APP Framework
- Hospital-wide, 30-day, All-Cause Unplanned Readmission (HWR) Rate for MIPS Eligible Clinician Groups
- Risk Standardized, All-Cause Unplanned Admissions for Multiple Chronic Conditions for ACOs.
- CAHPS for MIPS Survey
Making the transition by 2025
Quality Category Options
CMS has given participants the option of submitting both CMS Web Interface measures and eCQMs or CQMs in 2022 through 2024. This allows you to compare your performance and make improvements until you are required to make the switch in 2025.
2025 Quality Category Options
When you finally make the switch, remember that regardless of which reporting framework you choose, it’s all patients, all payers for all of your practices, 365 days of the year.
Understanding your Collection Type Options
Up until now, you have been using the CMS Web Interface measures (collection type). Since that option goes away in 2025 you must now pick a new collection type.
- eCQMs (Electronic Clinical Quality Measures)
- MIPS CQMs (previously called Registry measures)
- QCDR measures (Qualified Clinical Data Registry)
For your organization it will likely come down to two options for you. Should you submit eCQMs or CQMs? In general, eCQMs are less burdensome but require excellent data aggregation from all of your various practice EHRs. Compare that to CQMs which may be simpler to implement but could require a massive amount of manual abstraction.
CQMs vs eCQMs: Pros & Cons
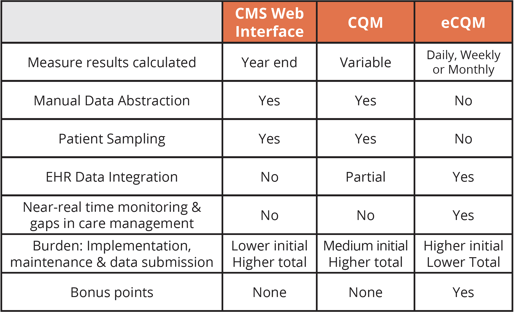
In our opinion the eCQM collection type is the way to go. Yes, it’s going to be a pain to bring together all of those sources of EHR data in the beginning. But once you get it set up, there’s no ongoing manual data abstraction.
Implementing eCQMs is the long-term play. Quite frankly, it’s the direction CMS is going, as made evident in the IPPS Final Rule where they committed to going completely digital by 2025.
They want measurement to be mostly electronic and not burdensome abstraction. So, while we recognize that every organization’s situation is different and eCQMs might not be the best fit, we encourage you to explore the eCQM option and see if it might work for you.
Finding a CMS Web Interface Measure Equivalent
If we’ve convinced you that eCQMs are the way to go, we wanted to provide you with a chart that shows the equivalent eCQM for each of the CMS Web Interface measures you’ve been submitting so far.
Making the Transition Easier
Our team has listed the equivalent eCQM ID on this chart below. We’ve also given you a colored guide. This is again just our opinion here, but as we’ve worked with clients to implement these measures over the years, we’ve found some to be easier than others. Green is easy, yellow is a bit difficult, and red is very difficult.
Also note, the three measures listed at the top in gray are your required measures if you choose or are required to report using the APP framework.
Medisolv MIPS PackageMedisolv Can Help Along with award-winning software, each client receives a dedicated Clinical Quality Advisor that helps you with your technical and clinical needs. We consistently hear from our clients that the biggest differentiator between Medisolv and other vendors is the level of one-of-one support. Especially if you use an EHR vendor right now, you’ll notice a huge difference.
• Blog: "3 Ways to Prepare for the CMS Web Interface Retirement" |






Comments