Patient Safety: Don’t Let a Case of Mistaken Identity Lead to Tragedy

Ever-changing patient and provider behaviors make it harder for quality managers to match medical records to the right patient. Avoid a case of mistaken identity with the right technology.
By: Denise Scott, M.M. RN-BC, CMHP & Roy Jones
“A case of mistaken identity set off an unexpected chain of events that (fill in the blank).”
If you were Shakespeare, you might fill in that blank with something like, “kept two star-crossed lovers from finding each other until it was almost too late.”
But, if you’re a doctor or nurse working at a hospital or health system, you might fill it in with “prevented two patients with similar names but with different medical conditions from getting the right drugs until it was almost too late.”
Matching patients to the right medical records is a growing challenge in healthcare, and it’s everyone’s responsibility to make sure an individual patient’s story doesn’t turn into an avoidable tragedy.
What patients don’t know can hurt them
Most patients are unaware that matching them to their medical records is an issue, and that it’s the very first marker of patient safety along the continuum of care. If they only knew how tenuous that match can be.
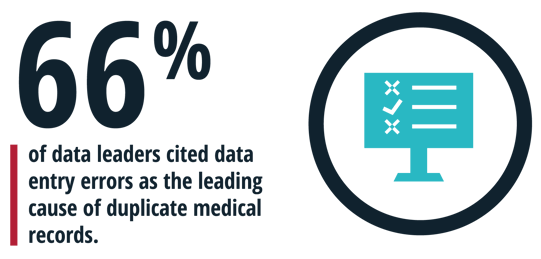
In February, for example, the eHealth Initiative published the results of a patient matching survey of 118 clinical data leaders at provider organizations and health information exchanges. All of the respondents acknowledged having at least some duplicate medical records in their EHR or information systems for the same patients. Data entry errors were the leading cause, cited by 66% of the data leaders.[i]
In March, the Department of Health and Human Services’ (HHS) Office of the National Coordinator for Health Information Technology released its annual report on the state of interoperability among general acute-care hospitals in the U.S. It said only 46% of hospitals engaged in all four aspects of interoperability in 2018. Those four aspects are sending, receiving, finding and integrating patient information with another provider outside of their health system.ii
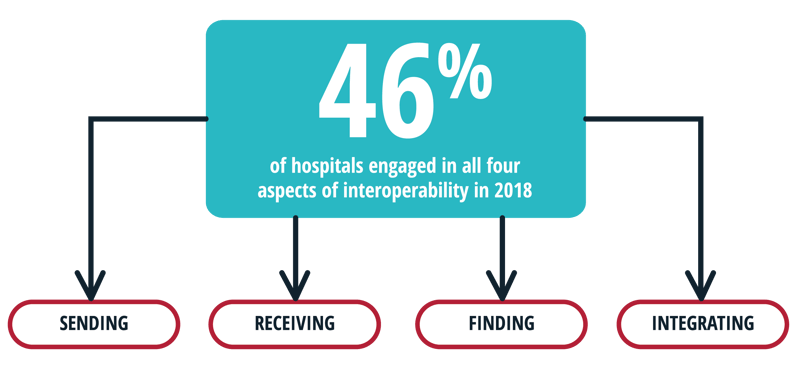
Asked about barriers to receiving patient health information electronically, 54% of the hospitals said it was “difficult to match or identify the correct patient between systems.” In other words, more than half of the hospitals in the U.S. have trouble using patient health data from other providers, because they can’t match it to the patient in their waiting room, exam room, emergency room, procedure room or hospital bed. That’s an effective plot for a scary Robin Cook novel. It’s not an effective way to provide optimum care to your patients.

A patient by any other name
The root cause of the struggle to match patients with the right medical records is the lack of an industry-wide standard on how to enter a patient’s name on their electronic medical record at the initial point of contact.
Is it last name, first name or first name, last name? Middle name or middle initial? Surname prefixes, suffixes or both? Date of birth, but which year format? Phone number with slashes or dashes? Spell out or abbreviate street addresses?
Another issue? Knowing which identifying patient information or data to include in the record. As long as there are different EHR systems built by different vendors and used by different providers, each provider may be entering patient names differently.
The lack of common patient information fields and formatting makes it difficult to match records electronically and match them to the same patient. That may not have been as important 20 years ago when most patients saw the same doctor, went to the same hospital, used the same name, kept the same phone number and lived in the same place for most of their lives.
But now consider that patients:
- Are more mobile and visit disconnected settings for primary-care services like retail clinics, urgent care facilities and retail pharmacies
- Go to different hospitals each time their insurance coverage changes
- Change their last names more frequently due to marriages, divorces and other civil unions and disseverments
- Change their phone numbers more frequently as they drop their land lines and regularly upgrade their smartphones
- Change their addresses more frequently as society becomes more mobile and people change jobs or lifestyles
- Are using mobile health apps and wearable medical devices that collect data and download it into their medical records
- Change their gender as gender reassignment surgery becomes more common and covered by health insurance plans
And consider that hospitals, health systems and medical practices:
- Use different EHR systems in different departments
- Switch EHR systems and vendors
- Merge with, acquire, partner and joint venture with other hospitals, health systems and medical practices each with different EHR systems
- Refer patients to different specialized services and medical specialists each with a different EHR system
The net effect of all this change is the creation of dozens (if not more) of medical records for the same patient as they interact with the healthcare system at different points in their lives.
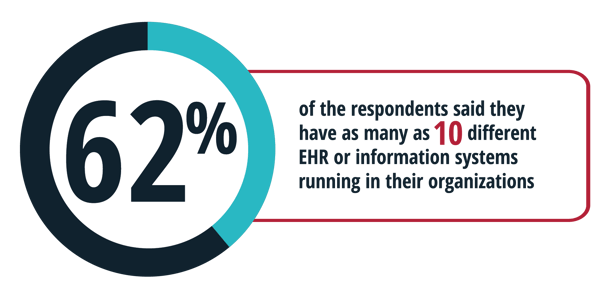
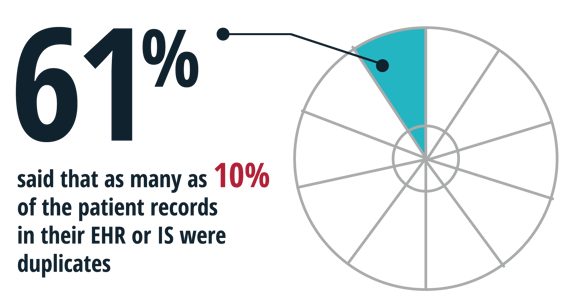
Sixty-two percent of the respondents to the eHealth Initiative survey said they have as many as 10 different EHR or information systems running in their organizations, each collecting patient information. Sixty-one percent said that as many as 10% of the patient records in their EHR or Information System (IS) were duplicates.
Appreciating the clinical and financial risks
In some cases, more is better. But that adage doesn’t hold true when it comes to medical records and the possible patients assigned to those records. Mismatched records and patients create a significant patient safety risk.
In fact, patient matching in EHR systems were among ECRI’s top 10 patient safety concerns for 2020.iii
“When matching is not successful, duplicate and overlay records are created,” the patient safety organization said in its March report.
Overlays are when someone documents one patient’s health information in another patient’s medical record. That’s not ideal when a clinician is reading a patient’s medical record to decide what drug to give, what test to order or what organ to remove. It’s especially detrimental when the wrong information stays in a patient’s record, compounding the initial mistake by creating additional patient safety risks in the future.
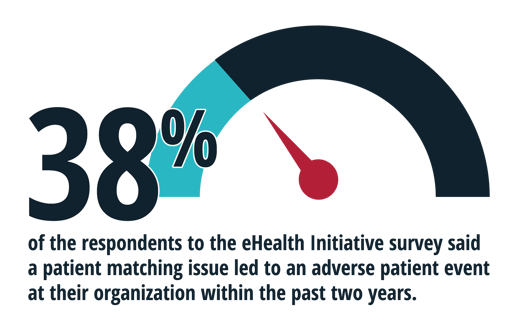
Thirty-eight percent of the respondents to the eHealth Initiative survey said a patient matching issue led to an adverse patient event at their organization within the past two years.
Patient matching issues can also mean having too little information. If diagnoses from other visits or lab results from other diagnostic tests don’t make it into the right record, it makes it harder for the clinician to treat the patient effectively.
Having too little information also makes it more difficult for providers to collect and report quality measures to value-based reimbursement programs like MIPS (Merit-based Incentive Payment System) and others that pay providers based on how well they meet those measures. Measures depend on clinical data extracted from patients’ medical records. If that data is wrong or missing because of matching problems, the measures calculation will be affected, and that could affect payment.
Implementing patient matching as a solve
So how can the industry solve this medical mystery? At a macro level, the answer is a national patient identifier. One patient, one number.
In June, the National Quality Forum (NQF) called for the nationwide implementation of what it called a “single-person identifier to match people to health records across all care settings.” The NQF made the recommendation as part of its “The Care We Need” initiative to improve the health system in the U.S. by 2030.iv
Such a single-person identifier “potentially minimizes inappropriate care and reduces medical errors,” the NQF said.
A patient in the emergency room today can’t wait 10 (or more) years for that to happen. So right now, that responsibility falls on individuals and technology.
Enter the widespread use of “defensible matching.” Here, software data electronically matches as many pieces of patient information as possible until your organization can defend its decision that a patient and a medical record are a match, or that two different medical records are a match for the same patient. That’s how we complete defensible matching for our clients using Medisolv software. We take the data from their EHR or multiple EHRs and match the patients in a defensible way to produce measures results for the client. That process typically starts with four data elements:
- First name
- Last name
- Date of birth
- Gender assigned at birth
If those four elements are a match, you can reasonably defend your decision that you have the right patient matched with the right medical records. If not, you must look for matches of other data elements, if they’re available, like social security numbers, phone numbers and addresses.
Technology can also help. You can deploy “standardizer” software that reviews patient records to determine the percentage of a probable match and standardize common words or abbreviations. Think of the digital prompt on your GPS or mailing address confirmation page when you buy something online. It’s the same algorithm.
Whichever patient matching protocols or quality assurance measures you implement, you must use them at every patient encounter along the entire continuum of care to ensure that you’re assigning the right clinical information to the right patient in their medical record.
Then (and only then) will your patients’ medical care be safely based on accurate and complete health information.
Learn more about Medisolv’s software capabilities here.
[i] “The State of Patient Matching in American: A 2019 National Survey.” eHealth Initiative. February 2020. https://marketing.nextgate.com/acton/attachment/3826/f-113c4b92-3369-4b94-8612-d57b2889e964/1/-/-/-/-/NextGate-eHI%20Patient%20Matching%20Survey%20Results.pdf?nc=1
[ii] “State of Interoperability Among U.S. Non-Federal Acute Care Hospitals in 2018.” Office of the National Coordinator for Health Information Technology, HHS. March 2020 https://www.healthit.gov/sites/default/files/page/2020-03/State-of-Interoperability-among-US-Non-federal-Acute-Care-Hospitals-in-2018.pdf
[iii] Top 10 Patient Safety Concerns 2020. ECRI. March 2020. https://www.ecri.org/press/diagnostic-errors-maternal-health-top-ecri-2020-patient-safety-concerns
[iv] The Care We Need: Driving Better Health Outcomes for People and Communities. National Quality Forum. June 2020. http://www.qualityforum.org/News_And_Resources/Press_Releases/2020/National_Quality_Forum_Releases_Task_Force_Roadmap_to_Normalize_High_Quality_Care_for_Every_Person_by_2030.aspx
STAY AHEAD OF THE QUALITY CURVEMedisolv’s Value Maximizer software, uses machine learning and predictive modeling to forecast your future years payments in the CMS hospital quality programs (HAC, HVBP, HRRP). Our simulation guides your team on how to optimize your performance to maximize your reimbursements. Here are some resources you may find useful. Blog: "Patient Safety Lessons Learned from the Aviation Industry’s Missteps" |



.png?width=352&name=BlogImage_State%20of%20IQROQR%20Survey%20(4).png)

Comments