What’s a Good Opioid eCQM Score?

Before we reveal the what, let’s talk about the why.
Why did CMS create an opioid eCQM that the federal agency is requiring hospitals to submit starting on Jan. 1, 2022? You, as a hospital or health system quality leader, can find the answer in the latest drug overdose figures from the Centers for Disease Control and Prevention (CDC).
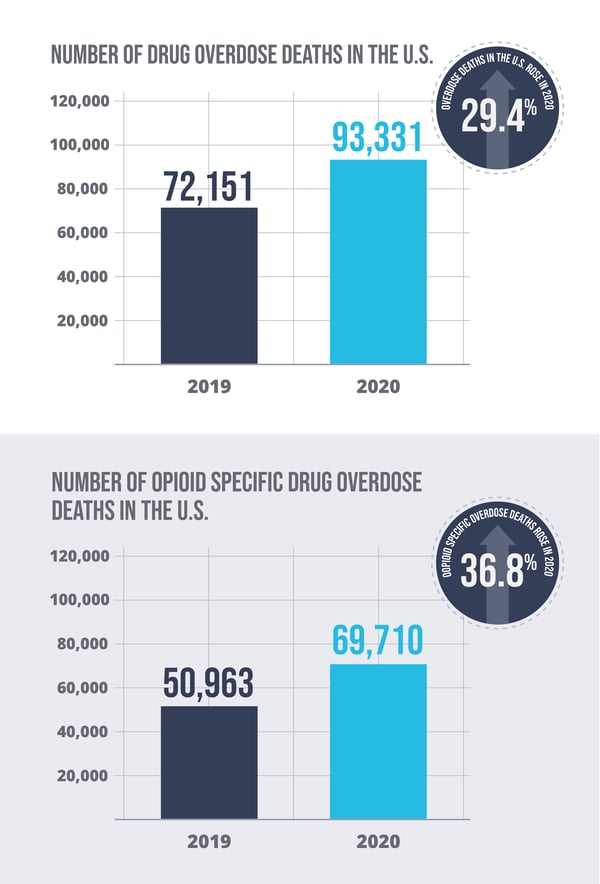
According to the CDC, the number of drug overdose deaths in the U.S. rose 29.4% in 2020—with 93,331 attributed deaths, up from 72,151 in 2019. Drug overdose deaths from opioids specifically jumped 36.8% to 69,710 in 2020 from 50,963 in 2019.
The opioid crisis is a persistent issue, and from the government’s perspective, everyone, including hospitals and health systems, needs to do their part to reverse the direction of these figures.
That’s why CMS created the new opioid eCQM, which is the share of your eligible inpatient population discharged with two or more opioid prescriptions, or an opioid and a benzodiazepine prescription. If your clinicians authorize more than the clinically recommended number of prescriptions, the odds of opioid addiction and patient overdoses go up.
As you know, hospitals and health systems like yours could voluntarily submit their opioid eCQM this year to CMS. Mandatory reporting starts in less than three months, and CMS will make each hospital’s results public on its Care Compare website. That’s why getting it right is so important.
Average and Median Opioid eCQM Scores
So, how do you define getting it right? What is a good opioid score?
Good is a subjective word, and what’s good for one hospital may not be good for another. But what we can tell you are the preliminary opioid measure scores from the eCQM benchmarking data we’ve collected this year from about 150 hospitals.
One thing to keep in mind when you review these measure performance rates is that this eCQM is an inverse measure, which means the lower the numerator count the better the performance rate. CMS has not provided hospitals with any percentage to shoot for, but they did make it clear that they don't expect hospitals to reach a 0% rate.
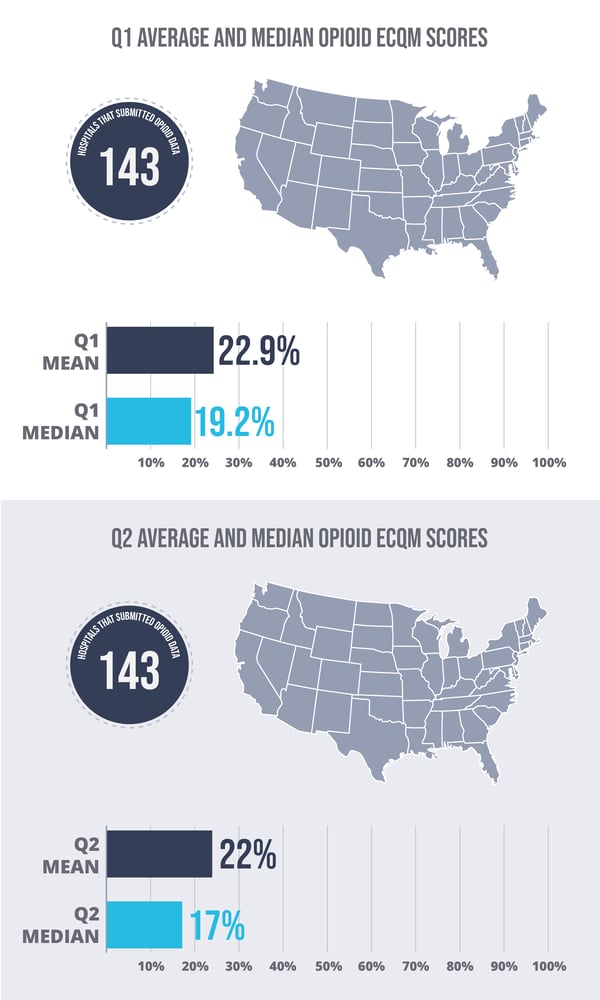
In the second quarter of 2021, we pulled in 143 of our hospitals' data into our benchmarking tool, and the scores ranged from 0%—no patients getting two or more prescriptions—to 100%, where every qualifying patient got two or more prescriptions for an opioid and/or a benzodiazepine. It’s important to note that the hospital with a 100% score had only two eligible patients, so you really have to look closely at the numbers.
The average score among the 143 hospitals that submitted Q2 data was 22%, and the median was 17%.
Those scores are slightly lower (better, in other words) than the Q1 2021 scores, when we compare data for 141 of our hospital clients. The average Q1 score was 22.9%, and the median was 19.2%. We will have Q3 data soon, and we’ll see if that downward trend continues as hospitals fine-tune their opioid eCQM data collection and reporting skills before the mandatory reporting period begins.
Find Out What Your Opioid eCQM Score Means
Most hospitals have been tracking and managing eCQMs for several years now, so implementing the Opioid eCQM, which is pretty straightforward, isn’t their biggest concern. it’s no surprise that the number one question we’re getting from our hospitals is not about implementation like we do for other, far more complicated eCQMs like the new ePC-06 measure from The Joint Commission. The question we’re getting about the opioid eCQM is, “Now what?”
This gets back to my earlier point about what’s good for one hospital may not be for another. As I mentioned, the new opioid eCQM is an inverse measure, which means the lower it is, the better it is—particularly during an opioid crisis.
To be clear, CMS says it does not expect a zero-performance rate for this measure. CMS understands that it will be medically necessary for some of your patients to be discharged on two or more opioid and/or benzodiazepine medications.
So, zero is not the goal. The goal is your lowest score possible, given your patient population and clinical service lines. That starts with knowing the benchmark score for your hospital. Are you above or below the mean and median scores for peer hospitals? Where do you rank?
Three Paths to Opioid eCQM Enlightenment
If your hospital has a higher performance rate (a negative thing in this case) than your peers, you need to ask why. Is it a mapping problem? Is it a clinical documentation issue? Or are some of your clinicians prescribing too many opioids for some patients who don’t need them, based on established clinical practice guidelines? In order to improve your score, you’ll need to understand the reason each patient qualified for the numerator and address the issue as appropriate.
If your hospital scores lower (better) than your peers, you also need to ask why, following the same information-seeking path: mapping, documentation and prescribing patterns. Any problems you find and fix along the way could push your score even lower, and that’s good.
If your hospital’s score is close to the mean and median scores of your peers, the worst thing you can do is nothing. The opioid eCQM is a high-priority measure for CMS, and it’s a highly visible measure for your hospital or health system. Driving that score as low as it can go while still being clinically appropriate will benefit your hospital or health system, and, most importantly, your patients.
Here are some additional resources that you may find helpful.






Comments