MIPS eCQMs vs Registry Measures: What’s the difference?
In the MIPS program, there are several different sets of quality measures that are available for the Quality category. You may have heard various terms thrown around: eCQM, Registry and QCDR. Depending upon your practice's situation, one of these "collection types" (as CMS refers to them) may be better suited for your needs. Typically most practices find themselves debating on whether they should use eCQMs or Registry measures for their Quality category data requirements. So what's the difference?
Today, we are going to review the difference between these two common measure types.
Before we begin, we have a note on terminology. CMS actually changed the language regarding these measures in the 2019 Quality Payment Program final rule. They changed "Registry" measures to "MIPS CQMs" - just to confuse us. But actually it should help to clarify what this measure is. And after you read this post, I think you will agree it does make more sense. The old Registry measures are very much what you think of when you think of traditional Clinical Quality Measures.
Now let's take a look at what makes up these two different measure types and why a clinician may choose one option over the other.
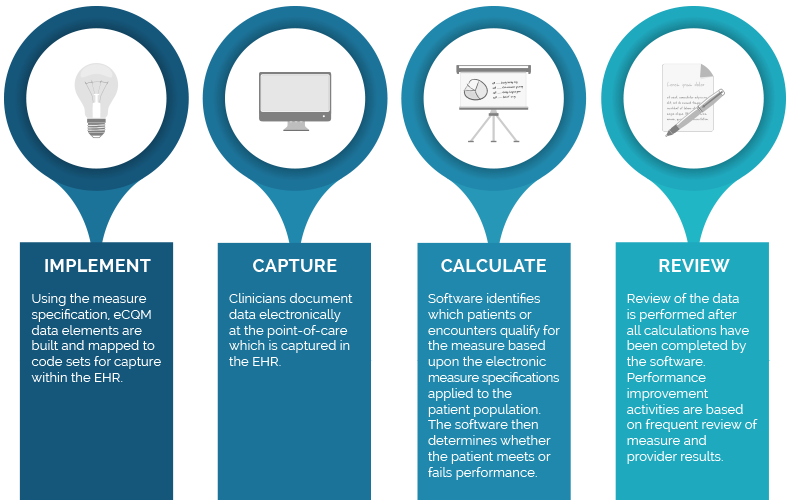
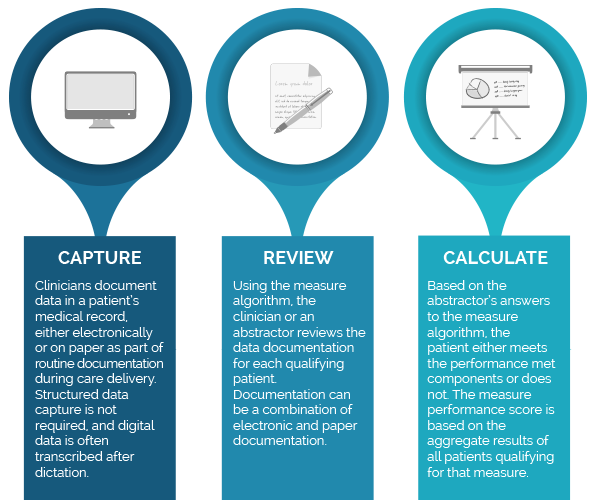
Capturing MIPS eCQMs vs MIPS CQMs (registry)
The main difference between eCQMs and MIPS CQMs is that eCQMs require structured data to be captured electronically, often at the point of care, while in most cases, MIPS CQMs have some level of additional manual data collection from the medical record often referred to as data abstraction.
For example, with MIPS CQMs, an abstractor can review the patient’s records (electronic and paper documentation) to assess whether the patient has passed or failed the measure. Even if a physician documented in a hand-written note that they prescribed aspirin for the patient, an abstractor could use that documentation to confirm that the patient did pass the CQM #0067: Coronary Artery Disease (CAD): Antiplatelet Therapy.
With eCQMs, the clinician documents in a structured field within the Electronic Health Record (EHR), usually as part of a clinical workflow ( e.g., ordering a medication using an electronic order entry system or documents a valid reason for not doing an expected intervention). This data is consumed by the eCQM calculation engine without additional manual data entry.
Below we summarize differences in both types of measures.
MIPS eCQM Process
MIPS CQM (registry) Process
Calculating eCQMs vs MIPS cqms (registry measures)
In addition to differences in data capture, the specifications and result calculations are also quite different.
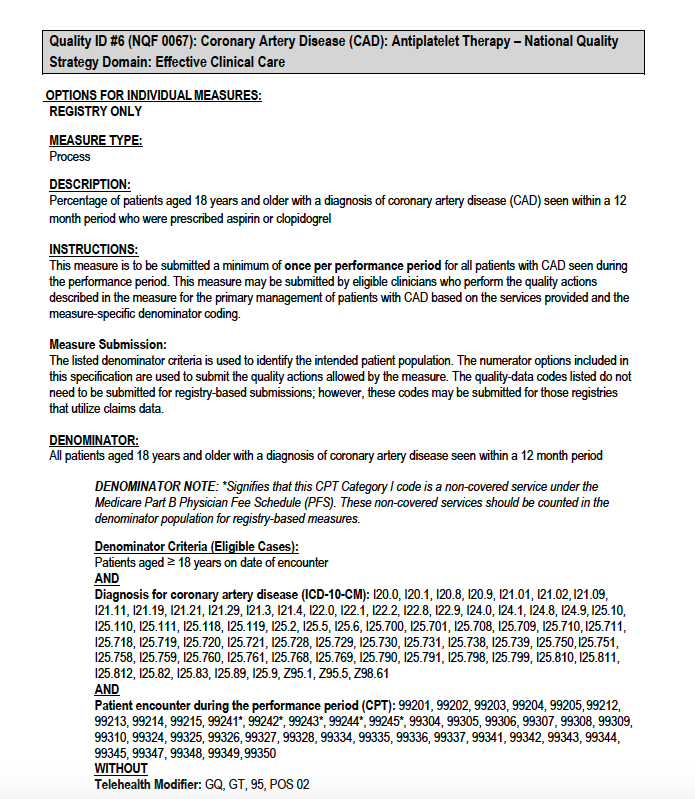
Comparing Specifications
The specifications for each measure differ significantly as well. Let’s take a look at the differences between the specifications at a very high-level.
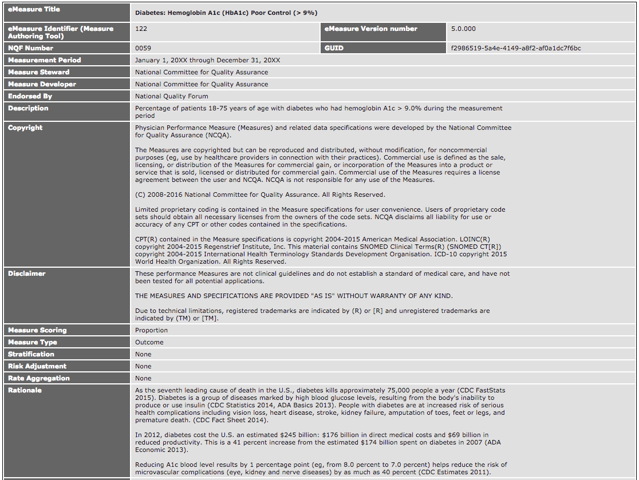
If you compare the descriptions, it all looks pretty similar. Each measure has a name, type, description and rationale.
|
MIPS CQM (Registry) Description Section |
MIPS eCQM Description Section |
| #0067: Coronary Artery Disease (CAD): Antiplatelet Therapy |
CMS122: Diabetes: Hemoglobin A1c (HbA1c) Poor Control |
 |
 |
Now let’s review the logic.
|
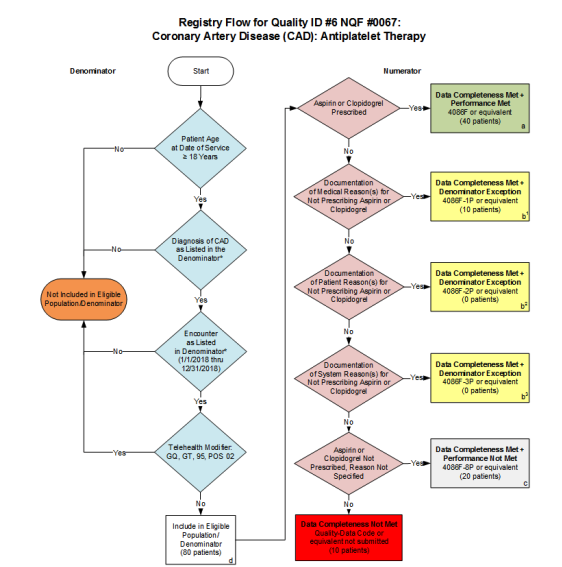
cQM (registry) specification Logic (Algorithm) |
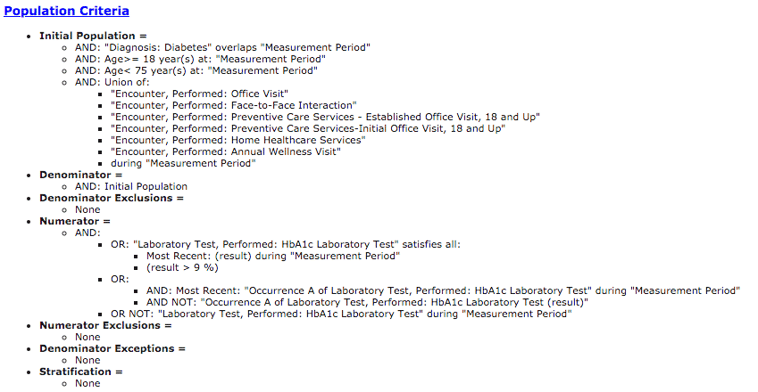
eCQM Specification Logic |
| #0067: Coronary Artery Disease (CAD): Antiplatelet Therapy |
CMS122: Diabetes: Hemoglobin A1c (HbA1c) Poor Control |
 |
 |
When you get to the logic, it starts to look different. With the MIPS CQM, a nice visual guides the abstractor through the measure. As you answer yes or no, it will lead you to the correct end result.
In the eCQM logic, you will see what’s called Boolean logic, which guides a computer through the measure logic and places patients into the appropriate result. Data elements in the EHR are mapped to codes. Each line you see in that logic will require a corresponding code to ensure that it’s captured correctly. If there isn’t a code present or if it’s the wrong code or if the documentation is not in the EHR, the patient may fall out of the measure.
Why would an Eligible Clinician choose eCQMs vs MIPS CQMs (registry measures)?
One of the most common reasons Eligible Clinicians choose MIPS CQMs is if there are not enough measures relevant to their specialty to meet the minimum reporting requirement. The down side is continued abstraction burden and lack of timely results to clinicians for performance improvement.
On the flip side, eCQMs (though they may be slightly more difficult to implement) provide near real-time reporting and have less costly ongoing maintenance.
There is another reason it might be easier to use the eCQM method. When you are submitting as a group, results are applied at the group level. Let’s say, in your group, you have three gastroenterologists and 12 primary care physicians. The primary care physicians could submit their eCQM results and the entire group would get credit based upon their performance. So if your gastroenterologists can't find measures that are applicable to them, your PCPs can submit their eCQM performance and you wouldn’t need to worry about your gastroenterologists because they would get credit for the PCPs' performance.
Other Quality Measure Types
You may have heard about the other ways to meet your Quality category requirements under the MIPS program. I’ll touch on them briefly here.
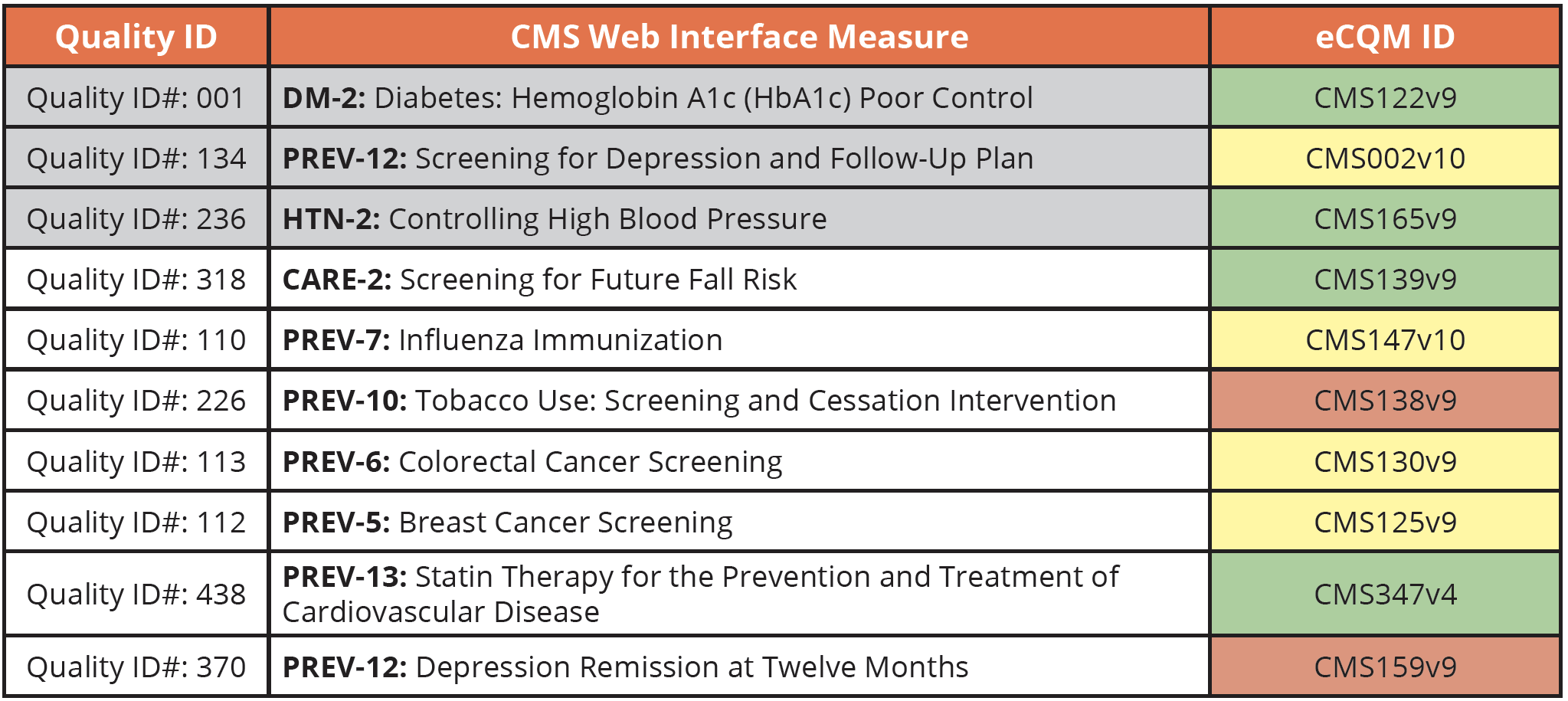
CMS Web Interface
Update: The CMS Web Interface measures will be sunset by 2022. If you previously submitted these measures you must now choose a different measure type. In most cases, you will need to choose either eCQMs or CQMs. The big change here is that you are going from a sampled list of 248 patients for each measure to all patients, all payers, across all practices.
For additional help, download our Guide to Transitioning from the CMS Web Interface measures.
Here is a cross walk from the guidebook to help you find equivalent eCQMs. This is just our opinion here, but as we’ve worked with clients to implement these measures over the years, we’ve found some to be easier than others. Green is easy, yellow is a bit difficult, and red is very difficult.
Also noted on this graph in gray are the required measures if you are an ACO that participates in the MSSP.
Qualified Clinical Data Registry (QCDR)
If you decide to report through a QCDR, you can choose from any of the approved QCDR measures developed by that QCDR. These measures are outside of the MIPS measure sets mentioned above. They are usually for very specialized Eligible Clinicians that cannot find appropriate measures in any of the other reporting methods.
What if I’m in an APM or ACO?
Are you in an Advanced APM or a MIPS APM? If you are in a MIPS APM or an ACO, you will still have to report your Quality measures, but your APM/ACO will provide you with a set of required Quality measures. While they are ultimately responsible for sending that data to CMS for you, they will likely have requirements for you to complete. So you should still be monitoring and improving your performance throughout the year for submission to your APM/ACO.
Another thing to note. Even though you are a part of an APM/ACO, you are still responsible for completing your other requirement in the Promoting Interoperability category.
I hope this quick summary of the differences between MIPS eCQMs vs MIPS CQMs was helpful. If you need help submitting your Quality data using eCQMs, MIPS CQMs or Web Interface methods, reach out to us today. We can help you with all of your MIPS reporting needs in every category.
Medisolv MIPS PackageMedisolv Can Help
Here are some resources to help you get started:
|

.png?width=352&name=2026%20Quality%20Reporting%20Deadlines%20Guide%20(1).png)



Comments