Best Practices for MIPS Year 3

Does anyone else feel like 2019 is flying by? Before you know it the summer will come and go and you'll be staring down Q3 thinking "I haven't even thought about MIPS yet." Don't let this happen to you! Now is a perfect time to start working on your provider's performance. Remember that in MIPS, performance counts; and for the Quality and Cost categories, that performance counts for 365 days of the year.
There's a lot to think about when it comes to MIPS reporting including measure performance, requirement changes and proper technology. That's why it's so important to avoid scrambling at the last minute by starting your MIPS prep early. Keep in mind that in addition to a greater risk and reward factor this year (-7% vs +7% reimbursement), you'll have to make sure that you implement the 2015 edition of CEHRT by October 1st to fulfill all of your category requirements. *Pause to breathe*

To help you gear up for another round of MIPS reporting, we've laid out the 2019 category requirements with a few tips to help maximize your performance and overall results.
Note: CMS made a few changes to your 2019 MIPS requirements in response to COVID-19. Changes are noted below. Read our blog, to learn more about the overall changes to quality reporting in response to COVID-19.
MIPS Scoring
Let’s start with a refresher on how CMS is calculating and finalizing your MIPS score for 2019. Take a look at the graphics below for the breakdown.
Category Percentages
Just as in 2018, there are four MIPS categories that will count toward your overall score in 2019: Quality, Improvement Activities (IA), Promoting Interoperability (PI, formerly Advancing Care Information) and Cost.
Unlike 2018 however, the percentage weight for the Quality category will decrease from 50% to 45%, while the percentage for the Cost category will increase from 10% to 15% this year. The weighting for the IA and PI categories will remain the same.

*Note: In response to COVID-19, CMS will not calculate Cost as a part of your 2019 score. If, however, you submit your other data by the extended deadline, CMS will add the weight of your Cost score to your Quality score.
Reimbursements
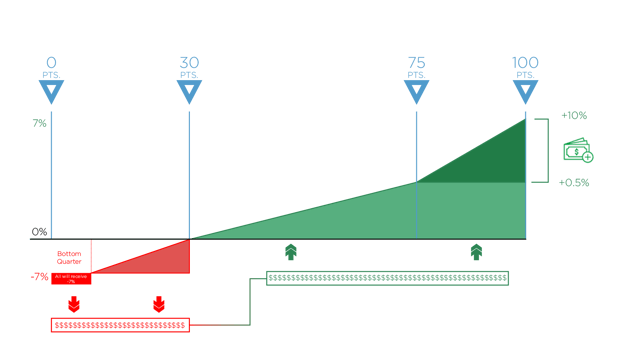
To avoid a penalty in 2019, you’ll need to score at least 30 points compared to 15 points in 2018.
And to qualify for the Exceptional Performance Bonus money that CMS sets aside for exceptional performers, you’ll need to score 75 points now as opposed to 70.
Remember, since MIPS is a budget neutral program, CMS will take all the funds from the negative payment adjustment and distribute them among those who met the performance threshold and achieved the positive payment adjustment. So, any Eligible Clinician or group who scores 30-100 points will be able to get some portion of these funds.
MIPS Tips by Category
Quality Category
 |
Requirements: Report a total of 6 Quality measures. Submit at least one Outcome measure unless there is not one available in your specialty measure set. If that is the case, you can report another High Priority measure in its place. |
 |
Max Category Points: 60 (or 70) points |
 |
Performance Period: 365 days |
TIPS FOR SUCCEEDING IN THE QUALITY CATEGORY:
- Make sure that all documentation is mapped correctly and that clinicians are using your EHR as intended.
- Review denominator cases to see why a patient is in the denominator only. Try to asses if it is a process issue or a patient issue. If it's a process issue, you'll need to work toward making that process better for providers and other clinicians.
- Try to submit more than one Outcome measure with high scores for bonus points.
- Submit using end-to-end electronic submission for bonus points.
- Based on your 2018 results, select one or two measures to improve for bonus points.
- Select measures carefully; avoid topped out measures for submission.
- If there are updates to your EHR during the year, ascertain that codes are not changed for key data elements.
Improvement Activities Category
 |
Requirements: Report a combination of IA measures (up to 4 measures) to equal a total score of 40 points. |
 |
Max Category Points: 40 points Groups with <15 participants or groups in a rural or health professional shortage area have their points doubled in this category. |
 |
Performance Period: Minimum of 90 days |
TIPS FOR SUCCEEDING IN THE IA CATEGORY:
- Select the measures that make sense for your organization and will provide you the best opportunity to improve over the course of 90 days.
- Document your starting point and share plans with clinicians.
- Touch base with clinicians for feedback on what is working and what is burdensome.
- Monitor results, modify actions and repeat.
- Explore Patient Centered Medical Home status. Ask yourself, "Is this the best for my organization?"
- In the past, CMS awarded bonus points to the PI category for any IA measures you submitted using the 2015 Edition of CEHRT. Note that there are no bonus points for these measures this year.
Promoting Interoperability (Advancing Care Information)
 |
Requirements: Report on six measures using the EHR technology certified to the 2015 edition of CEHRT. |
 |
Max Category Points: 100 points |
 |
Performance Period: Minimum of 90 days |
TIPS FOR SUCCEEDING IN THE PI CATEGORY:
- The PI category has changed the most in 2019, so be sure to MONITOR it consistently.
- Make sure you are submitting your best 90-day period.
- Get all of your staff involved in the Patient Access measure, which is worth 40 points of your score. Make it easy for the staff to provide access information to all patients and document that they received access.
- Keep clinicians invested in the ePrescribing measure. Ensure that their performance is on track with 2018 results or better.
- Go for the measures that give you bonus points; i.e. the Query of Prescription Drug Monitoring Program (PDMP) measure and the Verify Opioid Treatment Agreement measure.
HEALTH INFORMATION EXCHANGE (HIE) MEASURES:
- Support Electronic Referral Loops with the Sending Health Information measure- Be sure to include medications, medication allergies and problem list information in your QRDA file to receive the full 20 points.
- Support Electronic Referral Loops with the Receiving and Incorporating Health Information measure- This pertains to the referrals returned from another clinician or first-time patient. When providers see their patients after the referral is completed, ensure you upload the referral report and that providers reconcile medications, medication allergies and the problem list to comply with the numerator conditions for this new measure.
Cost Category
 |
Requirements: No actual submission needs to happen in this category. CMS will evaluate your performance on a total of 10 measures. CMS will evaluate your performance on the same two measures from 2017 - Total Per Capita Cost and Medicare Spending per Beneficiary. Additionally, there are 8 episode measures that include inpatient and procedural measures. |
 |
Category Worth: 15% 0% of total MIPS score (Cost score re-weighted to your Quality score in response to COVID-19.) |
 |
Performance Period: 365 days |
TIPS FOR SUCCEEDING IN THE COST CATEGORY:
- While these measures are calculated by CMS, you should analyze your results from the last two years (2017 and 2018) and look for cost-saving strategies.
- Inform clinicians about these measures and seek their input for cost savings and improvement.
General MIPS Tips
Involve Stakeholders
Keeping all of your stakeholders actively involved in the MIPS reporting process is crucial for success. Here are some things you can do to keep everyone involved and on the same page:
- Consider incentivizing improvement through clinician contracting.
- Provide clinicians with individual "report cards" for their 2018 performance so they can see where they need to improve.
- Provide monthly or quarterly reports during 2019.
- Post clinician results by measure for everyone to view.
- Continually educate clinicians on measure changes and requirements.
- Prioritize measure selection based on clinicians’ patient population and needs.
- Recruit clinician champions to work with clinicians whose measure rates are not meeting expectations.
- Make sure that the EHR works for clinicians.
- Involve the clinic staff to prompt clinicians prior to each visit.
- Recognize improvement with staff and clinicians.
- Ok and our biggest tip - don't do it alone! Of course this sounds disingenuous coming from a vendor, but truly. This stuff is difficult to sort through. With Medisolv you get software that gives you instant access to your results on a deep level and a dedicated expert who expands on all of these tips with you throughout the year. That's why our clients perform better than everyone else nationwide.
Reach out to us today and get ahead of the curve.
Medisolv MIPS PackageMedisolv Can Help Medisolv’s quality reporting software, ENCOR, is designed to meet your MIPS reporting needs. Our solution spans both the ambulatory and inpatient settings and includes consulting and submission services. Learn how we can help you successfully submit to the Quality Payment Program. Contact one of our MIPS professionals >>
|

.png?width=352&name=2026%20Quality%20Reporting%20Deadlines%20Guide%20(1).png)



Comments